A closer look at neurodegenerative diseases
Neurodegenerative diseases are disorders characterized by the progressive degeneration of the structure and function of the central or peripheral nervous system.
Dementia and Alzheimer’s disease
Facts and Figures
Brain changes
Diagnosis
Disease management
Dementia causes symptoms that affect memory, thinking, and social abilities severely enough to interfere with a patient’s daily life.
A lot of the diagnosis still depends on the report of relatives, who are often the first to notice changes in memory or personality and can describe changes over time.
Professor Clare Mackay, PhD, Associate Director, Oxford Centre for Human Brain Activity (OHBA), UK
SPECT exams should be made more accessible by reducing costs. It would be useful for screening patients with cognitive risks, to protect both themselves and a healthy society.
Jun Hatazawa, MD, PhD, Chief Executive Director, Japan Radioisotope Association
The likelihood of developing Alzheimer’s may be only one to two percent at age 65. But then it doubles every five years. Existing drugs cannot reverse the course of the degeneration, they can only slow it down. This is why it’s crucial to make the right diagnosis in the preliminary stages – when the first mild cognitive disorder appears – and to filter out Alzheimer’s patients.”
Andreas Papadopoulos, MD, PhD, Scientific Coordinator, Iatropolis Medical Group, Athens, Greece

Parkinson‘s Disease
Facts and Figures
Brain changes
Diagnosis
Disease management
Parkinson signs and symptoms can be different for every patient. Early signs might be mild and can even go unnoticed.

With objective assessment, we can predict the occurrence of movement disorder, which is useful for the prevention of Parkinson’s disease.
Hiroshi Matsuda, MD, PhD, Director, Cyclotron and Drug Discovery Research Center, Southern Tohoku Research Institute for Neuroscience, Japan

A normal SPECT DaT image (top) with the corresponding MR image (bottom). While DaT imaging is normally done with SPECT/CT, the striatum is better localized on MR images.

Multiple Sclerosis
Facts and Figures
Brain changes
Diagnosis
Disease management
Multiple sclerosis is a disease with unpredictable symptoms that can also vary in intensity. Different symptoms can manifest during relapses or attacks.

How to accelerate progress in diagnosis and treatment
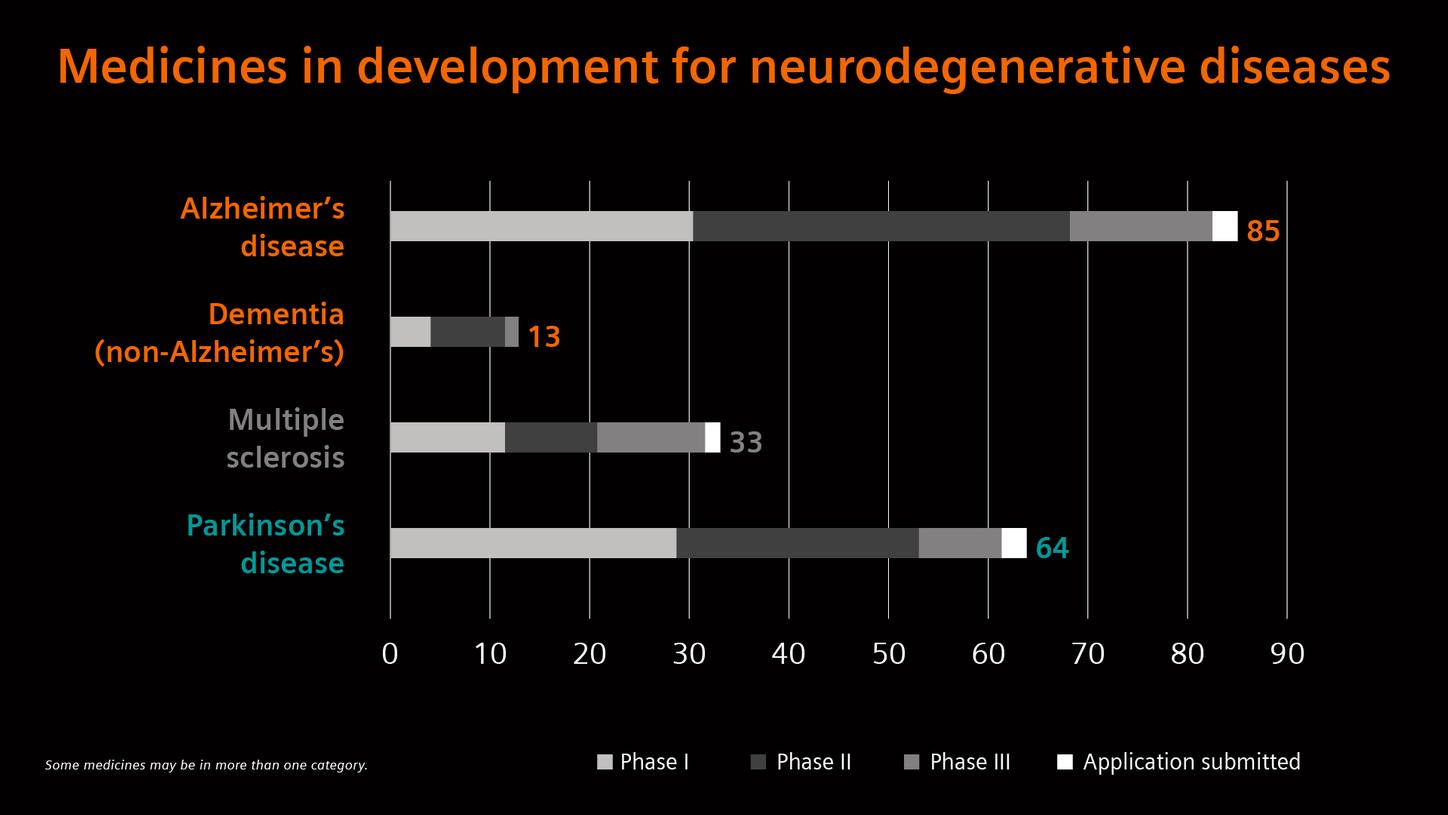
Given the limited diagnostic and therapeutic options for neurodegenerative diseases, researchers, and industry are pooling their strengths.
What lies ahead?
Looking at the near future - what could be possible next steps and developments?
The disorder starts 20 years before you see the symptomology. So, people have started to generate studies of healthy people, and follow them in time to identify early biomarkers. If you find the biomarker, or molecules in the blood, that reveals the first signs of the disease, you can try the drugs right away. Until we reach that point, it will be very difficult to find drugs.
Professor emeritus Adriana Maggi, PhD, University of Milan, Italy
1 Disability-adjusted life years (DALYs) measure overall disease burden, expressed as the number of years lost due to ill health, disability, or early death. They are also used to measure the impact of single diseases on a population.
2 Research mode on MAGNETOM Terra is still under development and not commercially available in the U.S. and other countries. Its future availability cannot be ensured.
The images are acquired with a MAGNETOM 7T which is for research only. All data shown are acquired using a non-commercial system under institutional review board permission.
The statements by Siemens Healthineers customers described herein are based on results that were achieved in the customer’s unique setting. Since there is no “typical” hospital and many variables exist (e.g., hospital size, case mix, level of IT adoption) there can be no guarantee that other customers will achieve the same results.All sources last accessed May 15, 2021
[1] https://www.alzint.org/about/dementia-facts-figures/dementia-statistics
[2] https://alz-journals.onlinelibrary.wiley.com/doi/abs/10.1002/alz.042236
[3] https://www.alzint.org/about/dementia-facts-figures/dementia-statistics
[4] https://www.parkinson.org/blog/raise-awareness/10-Interesting-Facts-About-Parkinsons
[5] https://parkinsonsnewstoday.com/parkinsons-disease-statistics[6] https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(18)30295-3/fulltext
[7] https://www.parkinson.org/blog/research/economic-burden-study
[8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7720355
[9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3770174
[10] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5476197/
[11] Gribkoff VK, Kaczmarek LK. The need for new approaches in CNS drug discovery: Why drugs have failed, and what can be done to improve outcomes. Neuropharmacology, 1 July 2017, volume 120
[12] Myszczynska, M.A., Ojamies, P.N., Lacoste, A.M.B. et al. Applications of machine learning to diagnosis and treatment of neurodegenerative diseases. Nature Reviews Neurology, 15 July 2020, volume 16
[13] Medicines in development. 2021 report: neurodegenerative diseases. Pharmaceutical Research and Manufacturers of America. 12 October 2021


























