“This technology is here to stay”
Associate Professor Tobias Granberg, MD, PhD, speaks about his expectations and experiences.
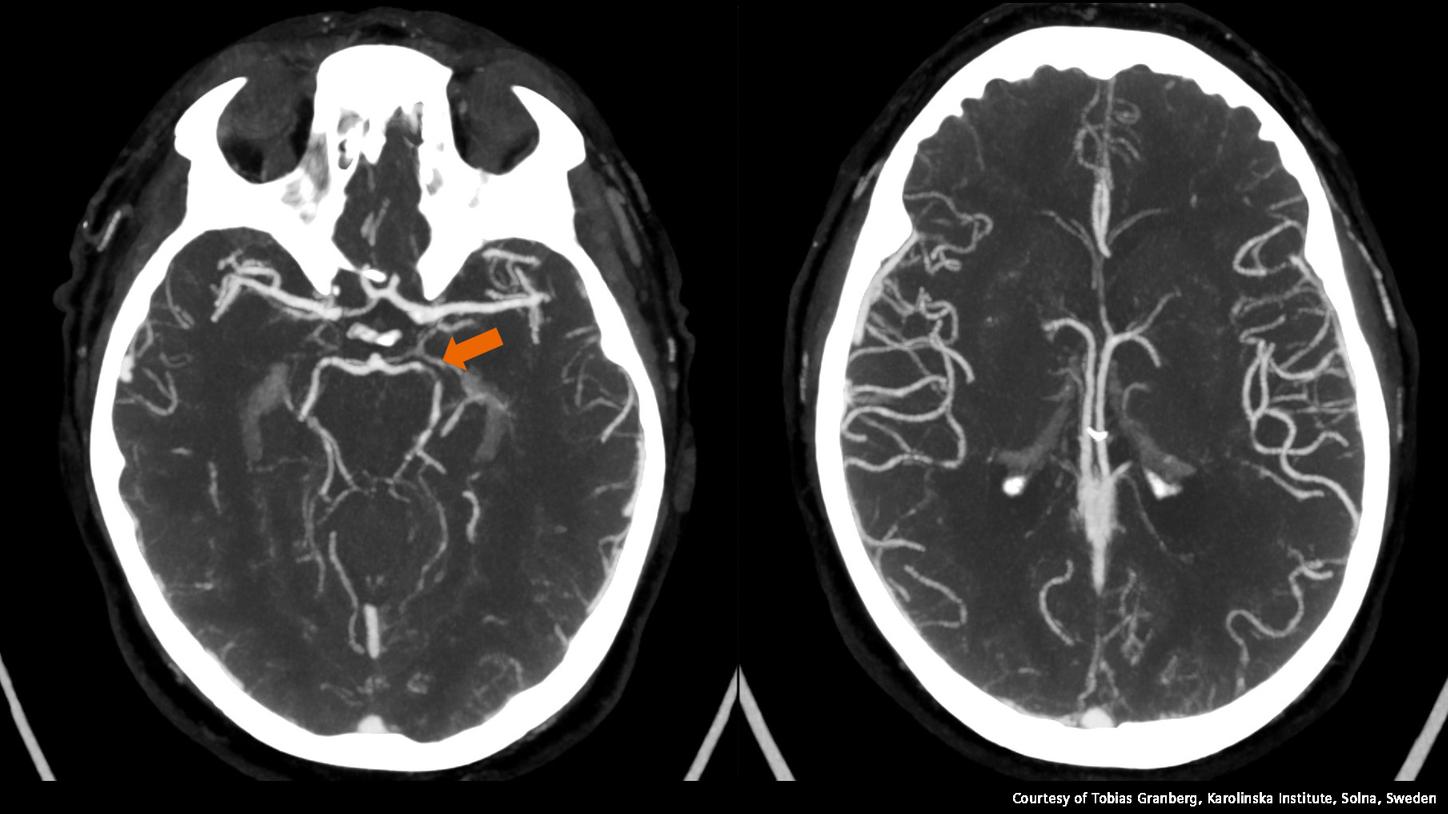
We’ve been able to reduce contrast agent dose by about 30 percent so far.
Associate Professor Tobias Granberg, MD, PhD, Department of Neuroradiology, Karolinska University Hospital, Stockholm, Sweden
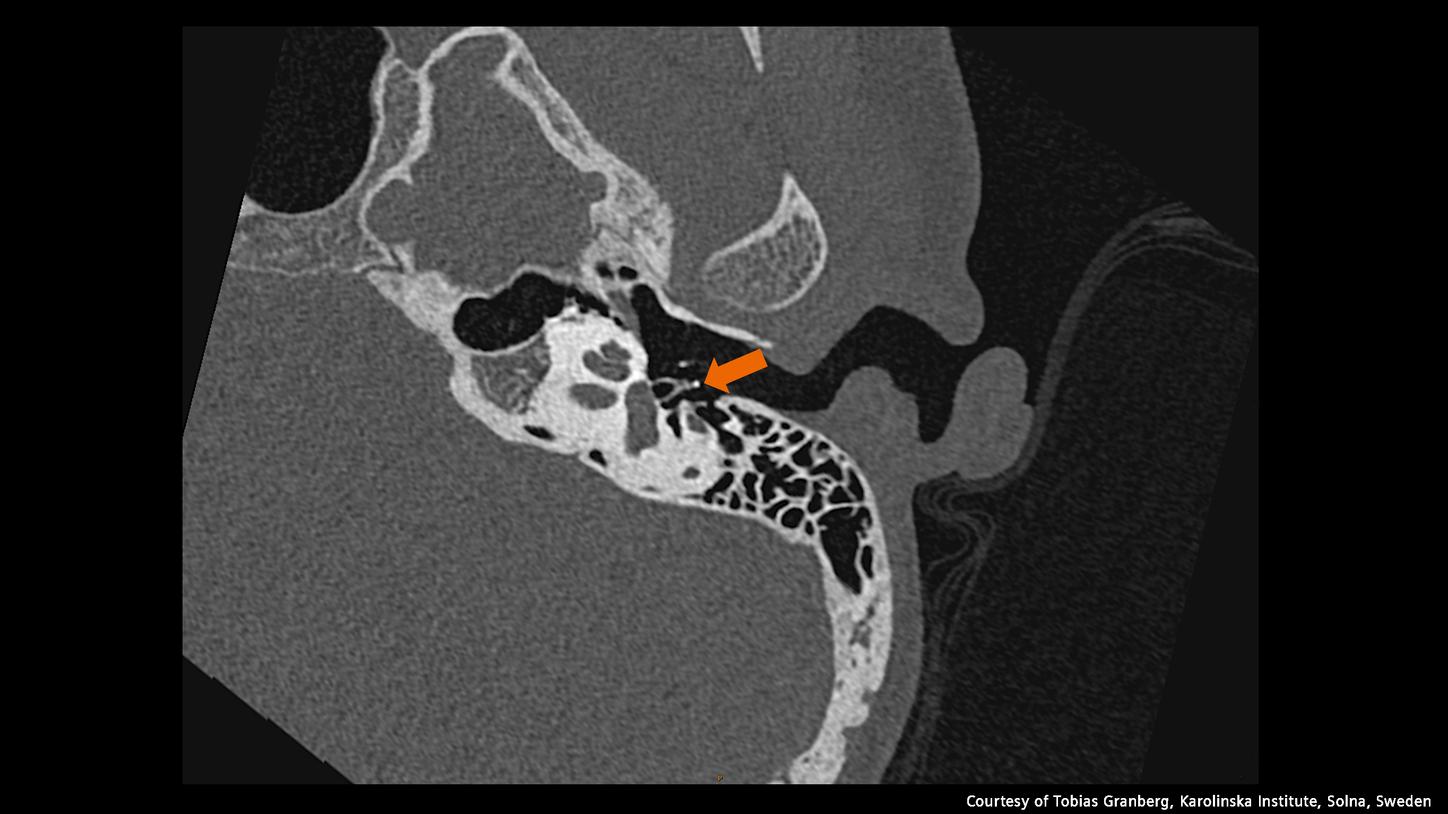
[Figure 1] Low-dose pediatric temporal bone scan (DLP 49) showing the stapes (arrow) in ultra-high resolution.
1 NAEOTOM Alpha is not commercially available in all countries. Its future availability cannot be guaranteed.
- The statements by Siemens Healthineers’ customers described herein are based on results that were achieved in the customer's unique setting. Because there is no “typical” hospital or laboratory and many variables exist (e.g., hospital size, samples mix, case mix, level of IT and/or automation adoption) there can be no guarantee that other customers will achieve the same results.