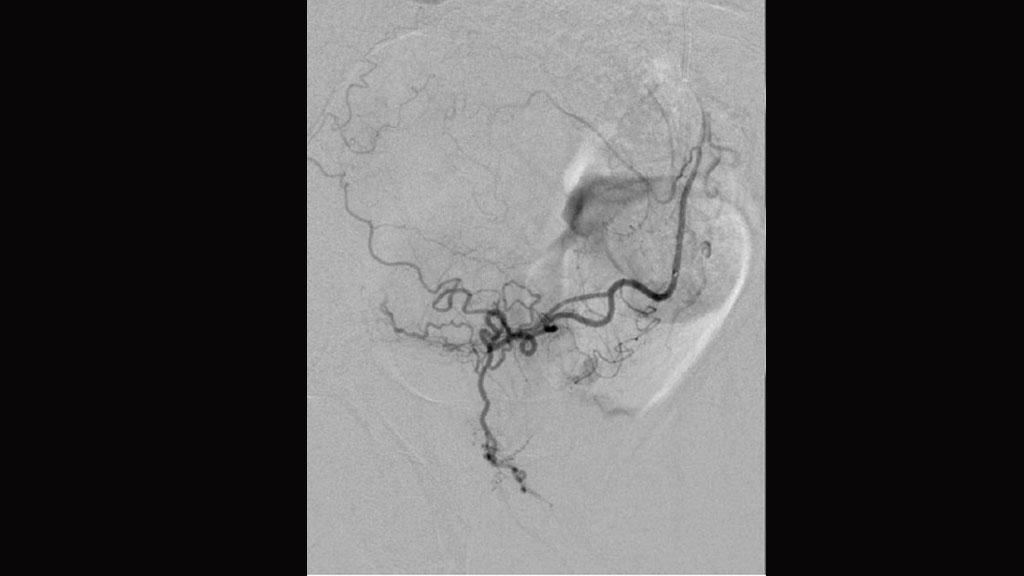
In 2018, prostate artery embolization (PAE) is probably on every interventional radiologist’s radar. The minimally invasive procedure now has an established safety and efficacy record, and has made rapid gains in becoming accepted as an alternative to surgery for patients with troubling urinary tract symptoms due to prostate enlargement. This article features renowned experts from Brazil, Europe, and Australia who help give a global picture of PAE in practice and trace its development.
Download your print version here.
Courtesy: Hôpital Européen Georges-Pompidou, Paris, France and Southampton General Hospital, UK
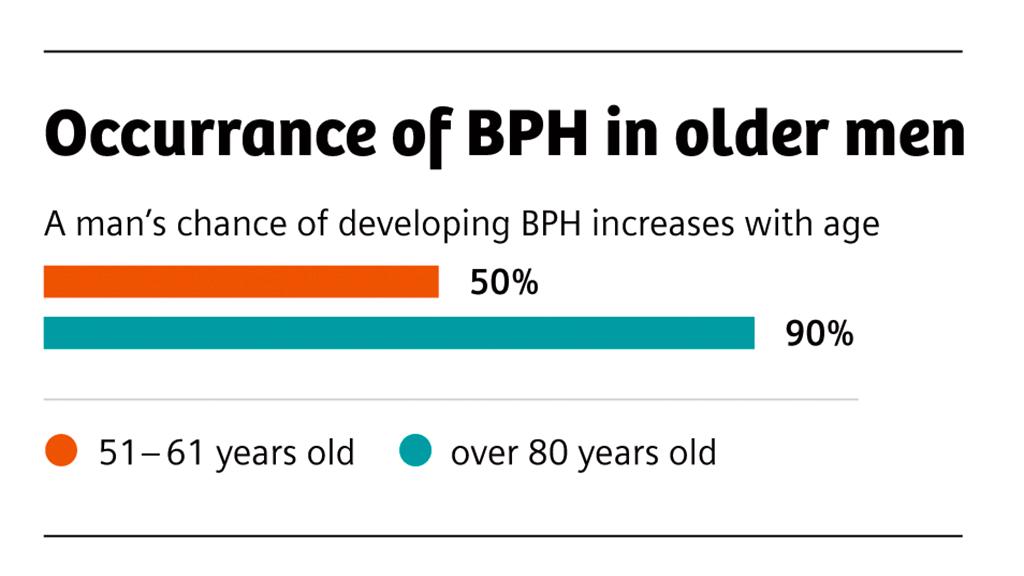
Urology Health, the official foundation of the American Urological Association, estimates that 50% of men between the ages of 51 and 60 and up to 90% of men over the age of 80 can develop benign prostatic hyperplasia (BPH). The exact cause of BPH is unknown. This enlargement of the gland leads to lower urinary tract symptoms (LUTS), including urinary frequency, nocturia, difficulty urinating, and incomplete bladder emptying. These symptoms can lead to a significant impairment to quality of life. The main types of treatments available are active surveillance and lifestyle changes, medical therapy, and surgery. Many experts view “PAE” as a unique treatment, a “bridge” between medical therapy and surgery.
The available clinical evidence has shown that PAE (which involves catheter-based, superselective delivery of embolic material to the arteries to block the blood supplied to the prostate with the aim of shrinking it) is nearly as good as surgical alternatives such as transurethral resection of the prostate (TURP) at decreasing the size of the prostate, lessening troublesome urinary symptoms and improving patients’ quality of life. Embolization scores over TURP in its safety profile and the length of stay in hospital for patients. One of the key reasons that men opt for PAE over surgery is that, unlike surgery, the minimally invasive procedure is associated with little or no retrograde ejaculation or sexual dysfunction after the procedure. Still, most interventional radiologist emphasize that PAE is a complex procedure that should only be offered to patients after multidisciplinary decision-making involving urology colleagues.
Francisco Cesar Carnevale, Associate Professor of Medicine, University of Sao Paulo, Brazil, is one of the pioneers of this new procedure and has worked strategically to gain widespread clinical acceptance of it. Since his first PAE cases in 2008, Carnevale has collaborated with urologists to put together the data needed to convince the Brazilian Federal Council of Medicine (Conselho Federal de Medicina, CFM) in 2016 that PAE can be used as a new, alternative treatment for symptomatic patients with benign prostatic hyperplasia.
Carnevale explains: “PAE is being used all over the world as an attractive alternative to medical and surgical treatments for patients suffering from BPH because it is a minimally invasive procedure, performed under local anesthesia, usually on an outpatient basis, with few, or no reported cases of urinary incontinence, retrograde ejaculation, or erectile dysfunction. That is why embolization has gained a lot of support from patients and from medical specialists even outside interventional radiology.”
In April 2018, the UK’s National Institute for Health and Care Excellence (NICE), which provides national guidance and advice to improve health and social care, decided that the current evidence on the safety and efficacy of prostate artery embolization for benign prostatic hyperplasia is adequate to support the use of this procedure on the National Health Service (NHS). NICE’s decision took into account the UK ROPE registry’s findings that PAE was safe and that it provided a clinically and statistically significant improvement in symptoms and quality of life for men with enlarged prostate.
Nigel Hacking, a consultant interventional radiologist at Southampton General Hospital, Southampton, UK, is the clinical lead for the UK ROPE registry. He and co-authors of the study emphasize in the leading urology journal BJU International in April that “PAE is an advanced embolization technique demanding a high level of expertise, and should be performed by experienced interventional radiologists who have been trained and proctored appropriately. The use of cone beam computed tomography (CBCT) is encouraged to improve operator confidence and minimize non-target embolizations”.
Efficient imaging modalities
Hacking states: “We perform our treatment planning on pre-interventional images. These are full high-resolution CT angiograms with maximum intensity projection (MIP) and 3D reconstructions to fully understand the anatomy of each internal iliac arterial tree with particular reference to the prostate arteries bilaterally and any important anastomoses. With regard to imaging modalities to assess the prostate anatomy, whilst ultrasound scans are typically used to assess prostate volume, CT angiography (CTA) is vital to accurately identify prostatic arterial anatomy. MRI is used if there is any concern about malignancy, but MR angiography has lower spatial resolution than CTA. From the CT angiogram we draw out the arterial anatomy on each side on to a proforma arterial map which is referred to during the PAE procedure itself.
“The spatial resolution of CTA is sufficient for assessment of vascular anatomy and even for detailed planning of catheter navigation and determination of therapy position of the microcatheter, as long as the technique is strictly adhered to.”
Rigorous training needed for PAE
“Training and being appropriately proctored is mandatory before offering PAE due to the highrisk nature of the intervention. It should be a step-by-step process,” explains Marc R. Sapoval, Professor of Radiology, Hôpital Européen George-Pompidou, Paris, France, who performed his first PAE in 2013. He has trained more than 100 interventional radiologists in the procedure.
“When you ‘see’ the first case, you understand the overall intricacies of the technique, and the difficulties but also the rewards that you get from helping patients with this procedure. Onsite training at our institution involves physicians who want to offer PAE coming into the angiosuite to observe three cases. They are positioned near the table and observe the entire preparation, flow injection, discussion, and DynaCT runs (CBCT performed on the angiography system). At the end of the day, this is a great starting point.
“The next step is to have a proctor onsite. This is where an expert comes to the trainee’s institution. You can then schedule two to three cases in a day and the expert can guide you through these. You can also attend one- or two-day courses that are available from many vendors, and there are now simulator-based training packages for PAE,” Sapoval says.
Vital to actively reduce radiation dose
“PAE is a complex procedure but radiation dose can be reduced for both the patient and operator,” reassures Goetz Richter of the Clinic for Diagnostic and Interventional Radiology, Katharinenhospital Stuttgart, Germany. Richter’s team has succeeded in significantly lowering the dose for both uterine fibroid embolization and prostate artery embolization. Siemens Healthineers has a Combined Applications to Reduce Exposure (CARE) system functionality for all relevant modalities.
“Before embarking on dose reduction strategies, first and foremost, operators need to achieve adequate expertise in the pelvic vascular anatomy. Once this is achieved, it is important to set a low frame rate for fluoroscopy (4/s); low frame rate for digital subtraction angiography (DSA; 1/s or 0.5/s) and the best possible collimations. Additionally, it is critical to avoid DSA whenever possible by using fluoroscopy overlay technology and to use a minimum number of oblique projections. Whenever possible, it is also useful to employ image fusion guidance. All these measures will result in dose reductions for both the operator and the patient,” Richter explains.
PAE in the angiosuite
Outlining the main requirements for performing PAE, Glen Schlaphoff, Director of Interventional Radiology, Liverpool Hospital, Sydney, Australia, identifies the first requirement as being a dedicated interventional unit that has access to nursing preoperatively, peri-operatively, and during recovery. “We then need an angiography machine, preferably an Artis zeego1, which allows total body coverage without moving the table. We have found this to be really important, having used a couple of different systems in the past. In my opinion, this robotic angiography system is highly suitable for PAE as it allows total body coverage from the radial artery to the groin, without having to move the table. This is crucial because there are very delicate catheter positions that can be altered if the patient moves. We also need access to a good workstation, rapid 3D assessment and rapid synchronization of datasets, both CT and angiography, during the procedure. A DynaCT run must be efficient. And we need very good arm support in the radial position,” he says.
Rapidly accumulating evidence for PAE, its approval for routine use by national regulatory bodies, and an explosion in interest from interventional radiologists in training opportunities lead experts to believe that PAE is “here to stay”.
About the author
Urmila Kerslake is a Bristol-based journalist. She is the Digital Education Lead and Senior Editor of the specialist quarterly newspaper, lnterventional News, with which the content of this article first appeared as part of a supplement.