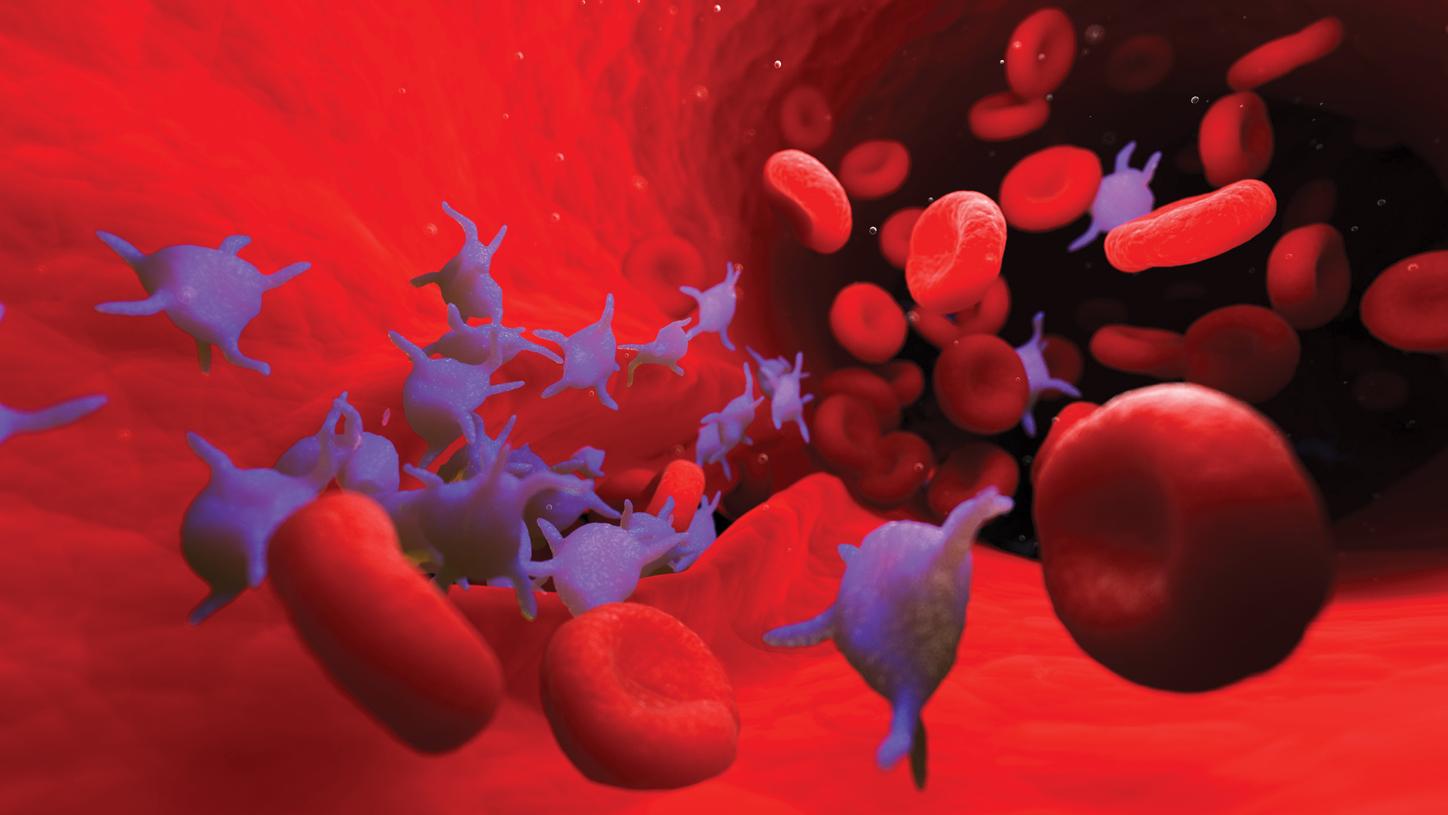
What is hemostasis?Why your body relies on a healthy balance of clotting and bleeding
Blood is a fluid that is circulated around the body through blood vessels. It performs many vital functions within the body, including defense and protection mechanisms, supplying oxygen and nutrients and regulating body temperature. Injuries such as a cut or bruise can damage blood vessels, which causes bleeding. In a healthy person, bleeding will automatically stop after a short time to prevent extensive blood loss. This function is called hemostasis.
Did this information help you?
The information provided herein represents a shortened and simplified explanation of hemostasis, hemostatic disorders and treatment. For more details, please consult scientific textbooks or publications.
General references for hemostasis:
Blanco A, Blanco G. Hemostasis. In: Blanco A, Blanco G, editors. Medical biochemistry. Academic Press; 2017. p. 781-9.
Reyes Gil M. Overview of the coagulation system. In: Shaz BH, Hillyer CD, Reyes Gil M, editors. Transfusion medicine and hemostasis (third edition). Elsevier; 2019. P. 559-64.
Cui, et al._JTH. 2020;18:1421. doi.org/10.1111/jth.14830
Klok FA, et al.Thromb Res. 2020;191:145. doi.org/10.1111/jth.14830
Llitjos, et al._JTH. 2020;18:1743. doi.org/10.1111/jth.14869
Middeldorp, et al. JTH. 2020. doi: 10.1111/jth.14888
Wichmann D, et al. Ann Internal Med. 2020;M20-2003. doi: 10.7326/M20-2003