History
Diagnosis
Virtual-monoenergetic images displayed at 65 keV revealed a lobulated, hypodense lesion located between the pancreatic head and body, measuring 19 × 21 × 17 mm. Multiple microcystic internal structures, with a maximum diameter of less than 4.5 mm each, as well as enhancement of the internal septa in the portal-venous contrast phase, were visualized. The pancreatic duct was not dilatated and showed no signs of lesion invasion. These CT findings suggested a diagnosis of a typical SCN without any worrisome features. Subsequently, the multidisciplinary team agreed with the patient on close follow-up examinations without the immediate need for surgical intervention.

Fig. 1: A coronal MPR image acquired on PCCT (Fig. 1a, 3 mm) shows a lobulated, hypodense lesion at the junction of the pancreatic head and body. Multiple microcystic internal structures (arrows) are clearly visualized. In a similar coronal view acquired 6 months earlier on a conventional CT (Fig. 1b, 3 mm), these microcysts are not depicted.
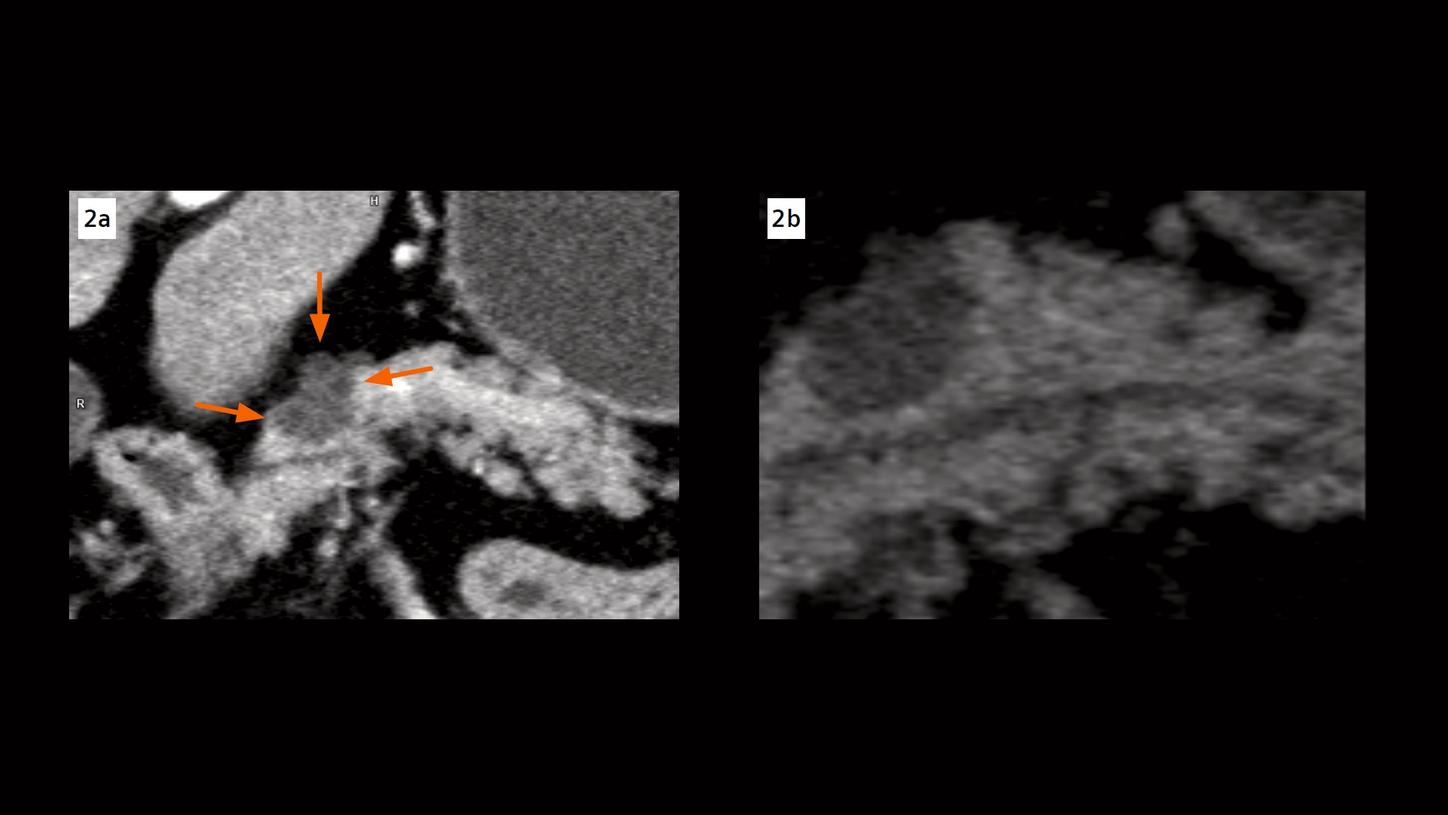
Fig. 2: Two enlarged views show the microcysts (Fig. 2a, arrows), and a clear separation between the lesion and the pancreatic duct, characterizing a typical SCN.

Fig. 3: Cinematic VRT images show the lesion (Fig. 3a, arrow) and the adjacent structures. An enlarged view (Fig. 3b) shows the microcysts in the lesion and the separation between the lesion and the pancreatic duct in three dimensions.
Comments
Pancreatic cystic neoplasm (PCN) is a collective term for pancreatic cystic tumors which have markedly different biological behavior. Main-duct-IPMN, for example, is considered a precursor lesion with a high risk of malignancy, while a SCN is classified as a benign entity with an extremely low risk of turning into invasive cancer. In the management of patients diagnosed with PCNs, high-end imaging with CT, MRI or EUS plays a central role. The goal is to provide accurate diagnosis in order to avoid unnecessary surgery on the one hand side, and to prevent delayed diagnosis when a precursor lesion has already progressed into invasive cancer. [1–2] Due to the increased availability and improved image quality, the probability of detecting PCNs has increased. [3-5] However, in some cases, differential diagnosis of PCNs can still be challenging.
This case is performed on a NAEOTOM Alpha, a newly developed Dual Source CT scanner with photon-counting detectors (QuantaMax™), providing energy-resolved CT data with inherent spectral information at improved spatial resolution and tissue contrasts, without electronic noise. [6] The spectral data is available in all routine scans, allowing for an easy switch of image display at different monoenergetic keV settings for an optimal image visualization. The images acquired during the portal and venous phases, which were traditionally displayed at 70 keV (equivalent to a standard 120 kV acquisition), now are routinely displayed at 65 keV, set as the standard energy level for an optimal visualization of the contrast-enhanced soft tissue structures because of the increased iodine contrast compared to 70 keV. The combination of the absence of electronic noise and the missing down-weighting of the lower energy X-ray photons further increases the iodine contrast-to-noise ratio (CNR), improving the image quality at low-energy display for routine diagnosis. Images are routinely acquired at 0.4 mm slices and reconstructed with a sharper kernel of Br44, providing increased spatial resolution compared to conventional standard abdominal CT. As shown in this case, owing to the improved CNR and the spatial resolution, the detailed visualization of the microcystic internal structures, the enhancing internal septa in the portal phase and the clear separation between the tumor and the pancreatic duct, help the radiologists make a confident differential diagnosis on PCNs, preventing unnecessary surgical interventions and potential complications for the patient.
Examination Protocol
