Partnering to deliver your vision
Siemens Healthineers is working closely with the NHS to deliver Community Diagnostic Centre (CDC) excellence, with efficiency, scalability and improved patient care at its core.
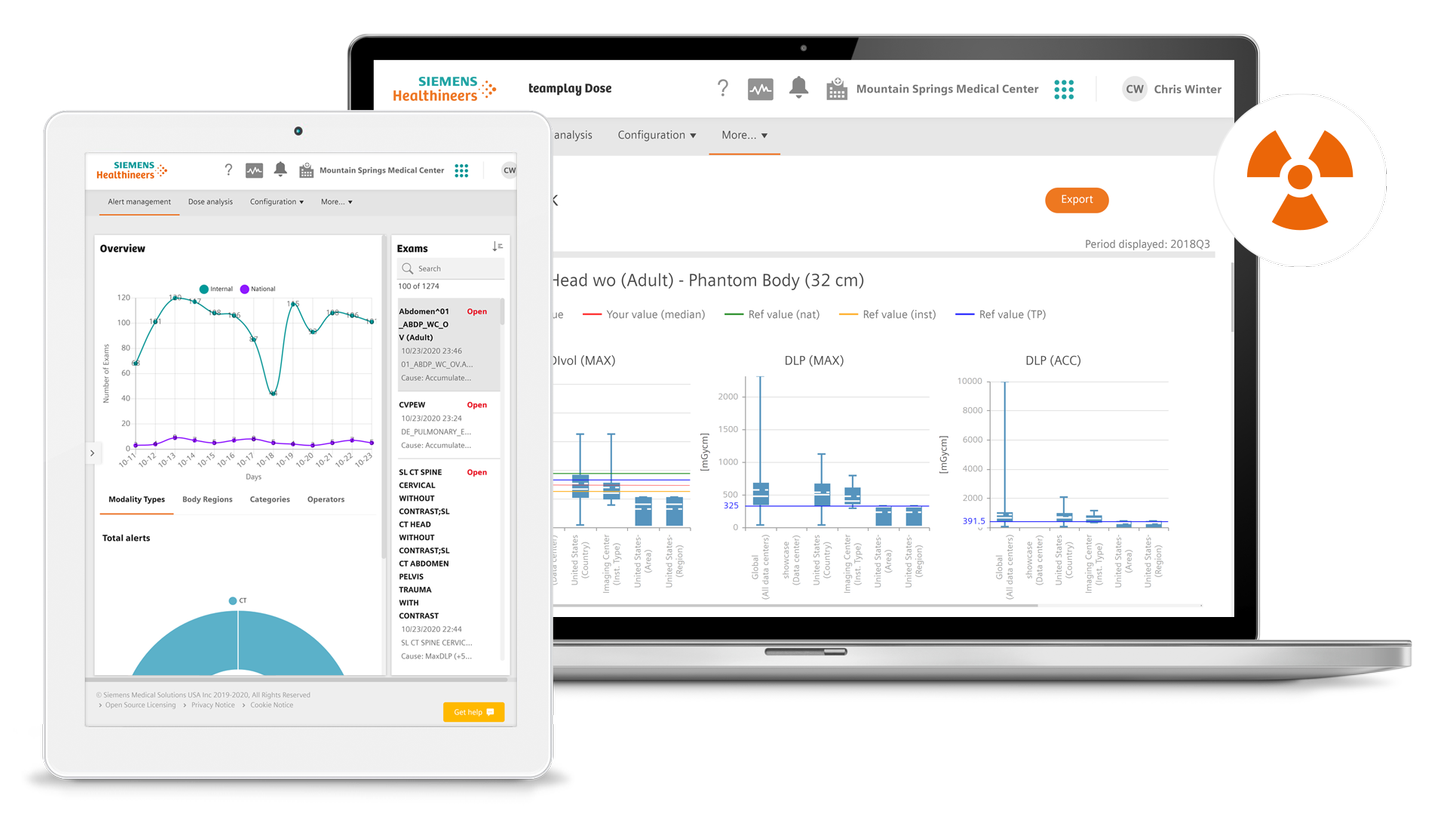
From design and planning to equipment provision, digitalisation to workforce planning, we can help to perfect processes throughout. As a trusted partner, we help to piece these together and deliver your vision for community diagnostics in a sustainable and cost-effective way.
We can also combine our products and services in financially innovative and flexible-term Value Partnerships.