Enabled by molecular imaging technology, theranostics using a PSMA-targeted radioligand therapeutic agent has the potential to enhance and prolong life for prostate cancer patients such as John. “I was able to feel more of myself. It was remarkable,“ he says.
Photography by James Farrell
When John was first diagnosed with prostate cancer 15 years ago, his level of prostate-specific antigen (PSA) was 650. Within in a week, it jumped to 1350, and his prognosis was bleak. “I was told that I would have from three months to three years, possibly, if I had decent treatment,” the 78-year-old recalls.
After beginning chemotherapy, the treatments soon fell into a familiar and disturbing pattern: the benefits of each round of chemotherapy would ultimately be outweighed by the side effects he experienced. Over time, his options became limited, and eventually he was offered hospice care. Theranostics changed the trajectory of his disease and his life.
What is theranostics?
Theranostics is an innovative form of personalized therapy that focuses on both the accurate selection of patients and providing them with targeted radioligand therapy to improve their prognosis.1 Theranostics refers to structurally similar diagnostic and therapeutic agents that share a molecular-specific target. Molecular targets are proteins on the surface of cancer cells and where the radioligand will bind. Throughout the theranostics process, molecular imaging techniques are used to identify, personalize, and monitor therapy response. Pharmaceuticals, such as radioligands, are used to target and treat specific areas.2 A radioligand is made up of a radioisotope that damages cancer cells and a target ligand that binds to specific markers on cancer cells.
“The concept of theranostics has been around for decades, but it’s really become actionable and exciting now because there are several prospective clinical trials showing a huge benefit,” says Joseph R. Osborne, MD, PhD, chief of Molecular Imaging and Therapeutics, and professor of radiology at a leading academic institution’s hospital in New York City, USA.
A targeted, personalized approach
A targeted, personalized approach
Radioisotopes of sodium iodide have long been used to diagnose and treat thyroid cancer, but Osborne notes that the recent development of theranostic agents that bind to prostate-specific membrane antigen (PSMA)—the antigen that is overexpressed in 90% of prostate malignancies3—has resulted in a significant expansion of the number of patients who can benefit from theranostics. Prostate cancer is the second most common cancer in men and the third leading cause of cancer death in men in the western hemisphere.4
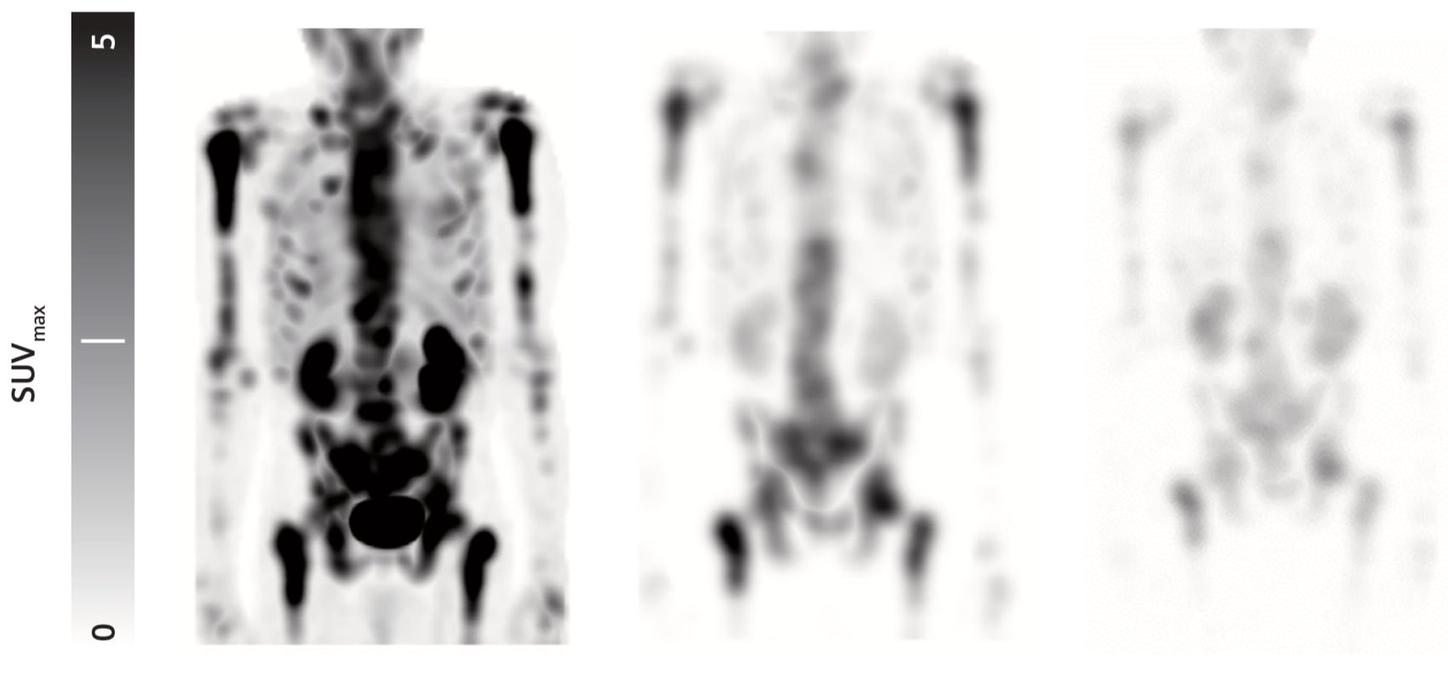
With theranostics, patients are injected with radioactive isotopes linked to molecules that bind specifically to tumors. A PET/CT scan may be used to localize tumors within patients and also to assess how much of the radioisotope tumors take up. Once this targeting step is completed, the diagnostic isotope is replaced with a therapeutic agent that kills cancer cells by delivering radiation directly to tumors. This targeted, personalized approach has the potential to reduce side effects for patients and improve outcomes.
Patient’s theranostics care pathway
Patient’s theranostics care pathway
The theranostics care pathway for the patient involves a series of steps and a range of laboratory diagnostic and imaging modalities. Beginning with patient selection, additional steps include personalized treatment, therapy response monitoring, and follow-up and survivorship monitoring. Read on to follow John along the theranostics care pathway.
Diagnosis and
patient selection
Diagnosis and patient selection
Patients with metastatic castration-resistant prostate cancer (mCRPC) who have been treated with androgen receptor (AR) pathway inhibition and taxane-based chemotherapy qualify to undergo prostate cancer radioligand therapy. In order to qualify for a prostate cancer radioligand therapy, patients must undergo a PSMA-ligand PET/CT to confirm PSMA expression in tumors. Based on the results of his PSMA PET/CT scan and his no-longer-successful hormone and chemotherapy treatments, John was eligible for theranostic treatment. After discussing it with his wife Mary and Osborne, he decided to undergo treatment.
“I was very weak when I came in to see Dr. Osborne, and we decided that this would be a good alternative,” he says. “There were six treatments, six weeks apart, and that was appealing to me because I had time in between.”
Personalized treatment
Personalized treatment
A patient receives pesonalized treatment based on molecular imaging with the diagnostic targeted radioligand to determine if the patient can benefit from a therapeutic radioligand. John began his treatment in April 2022. He experienced some nausea and vomiting after his first treatment, but those side effects quickly abated.
Mary was surprised to see him making breakfast the morning after his first treatment. “I couldn’t believe it,” she recalls. “He said, ‘Mary, would you like some breakfast?’ And I said, ‘Well, of course!’ He was very energetic, and we even have video of him dancing in August after his second treatment at our grandson’s party. And I mean he is dancing,” says Mary emphatically.
Therapy response monitoring
Therapy response monitoring
Monitoring response to therapy continues throughout the treatment regimen. John‘s physicians monitored his therapy response throughout his six treatments, which soon became an almost comfortable routine. He drove himself to the hospital, greeted staff, had his blood counts checked, and underwent infusion and then post-infusion quantitative SPECT/CT scanning.
John recalls that when his treatment first began, each visit to the hospital took between four and five hours. These visits combined scanning and infusions. As his treatment progressed, his physicians separated his treatment and post-imaging quantitative SPECT/CT over separate days to reduce the time he needed to be at the hospital in one sitting. Regardless of the protocol they used, he felt well enough to drive himself home.
“Dr. Osborne and the whole staff made me feel comfortable and genuinely cared about,” he says. “I walked in for my third treatment and they said ‘How do you feel, John?’ and I did a little jig. They all laughed at that, and it was indicative of my improvement.”
“I walked in for my third treatment and they said ‘How do you feel, John?’ and I did a little jig... It was indicative of my improvement.”
Follow-up and
survivorship monitoring
Follow-up and survivorship monitoring
Imaging and laboratory diagnostics play a vital role in post-therapy monitoring and follow-up. John says that in addition to increases in physical stamina—like his ability to climb stairs without becoming winded—he soon began to notice an improvement in his mental and emotional state. “It has a psychological effect on you to feel like you’re unable to do anything, and your self-worthiness gets so low,” he says.
He is now back to everyday tasks that he simply did not have the energy for before, like paying the bills, and he has even been able to travel again. He continues to see his physicians for regular follow-up and monitoring, and he and his wife both emphasize how grateful they are.
John and Mary’s experience
John and Mary’s experience
Theranostics has enabled John to return to a level of functioning that was almost inconceivable prior to his treatments. He and Mary urge families in similar situations to seek out the care they need.
“If I could give advice to anyone, I would say do your due dillegence,” John says. “Also, the thinking starts to shift as you receive these treatments, and you begin to hold on to those positive affirmations and ways of thinking about yourself in a greater way. “ When asked about her thoughts now that John is feeling stronger and has energy to do things again, Mary adds, “Being thankful and having gratitude is a very powerful thing.”
About the Author
More information