Ethan Colliver, DO, shares his insight and clinical experience using SPECT/CT in the detection and diagnosis process, and why he feels the utilization of nuclear medicine may result in more targeted and effective treatments.
Data courtesy of Valley Sports and Spine Clinic, Blacksburg, Virginia, USA
I was introduced to the use of single-photon emission computed tomography (SPECT/CT) during my Physical Medicine and Rehabilitation (PMR) residency training at the University of Utah from 2005-2008. In my 10 years of practice as a musculoskeletal PMR physician, I have often relied on the use of SPECT/CT.
The use of imaging in a musculoskeletal PMR practice is essential to gathering data that correlate with the patient’s history and physical exam findings in order to determine a definitive diagnosis. In the appropriate patient, SPECT/CT can allow the physician to localize pathology to a specific area, which is critical in guiding interventions and treatment. While established imaging methods such as X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) show anatomy, SPECT/CT is a hybrid of functional and structural imaging.
“SPECT/CT offers efficient identification of the pain generator, due to degenerative changes, ultimately reducing unnecessary imaging, invasive procedures, and potential risk caused by those procedures and surgeries.”
Functional imaging provides information on the physiological properties rather than the structural properties of the musculoskeletal system. This is the essence of functional imaging. Molecular imaging addresses the characterization and measurement of biological processes at the molecular and cellular level and is generally the prerogative of positron emission tomography (PET) and SPECT imaging.1
With SPECT/CT bone imaging, the radioisotope technetium-99m (99mTc) is attached to a phosphonate-bisphosphonate ligand and will be absorbed at higher rates where there is rapid bone metabolism. As the radioisotope decays, it will be detected by the gamma camera, allowing the localization of different areas of metabolic rates within the bone. Rapid bone metabolism is indicative of fracture, cancer, inflammation, and degenerative joint disease.2
How SPECT/CT helps my practice
While the CT allows the practitioner to see anatomy, the SPECT allows you to see the functional activity of the bone. The combined components and resulting images are used to help guide the diagnosis and treatment plan in my clinical practice. However, not all SPECT/CT scanners are created the same. The CT component should acquire images of diagnostic quality in order to localize the pain generator effectively. Factors to consider include: number of slices, rotation speed, pitch, and flexibility to fully utilize CT and have the best clinical results. The ordering provider may also need to evaluate the signal of the SPECT/CT component, as the received images can have the SPECT/CT signal turned up too high or too low, which can limit the ability to detect pathology from background noise.
Consider, for example, the 17 joints in the lumbosacral region. A patient can have an X-ray that shows multiple areas of arthritis in their lumbosacral region of the spine. However, the presence of arthritis does not predict the presence of pain. SPECT/CT may show that only one or two of those joints may be biologically active. This specificity can allow me to steer my interventions and treatment to areas of increased activity, while limiting unnecessary injections and procedures.

The complication rates of injections and surgeries have been well documented in the spine pain population. Dr Palmer wrote “by 2010, more than 2.2 million lumbar ESIs were performed yearly in Medicare patients. Facet injections surged 147% from 1993 to 1999 and increased another 300% from 1998 to 2006.”3 One paper reported an overall complication rate of 2.4% in lumbar epidural steroid injections, with the majority being minor or self-limited.4 Additionally, many case reports and series describe major complications and death occurring from spinal injections. Moreover, it should be noted that the reported complication rate of lumbar decompression and decompression with fusion surgery is 15%.5
Therefore, the decision to attempt spinal injections or surgery should not be taken lightly, and every attempt should be made to limit the exposure to these procedures. From 1994 to 2004, for example, there was a 307% increase in utilization of lumbar MRI images in the Medicare population.6 Due to the lack of physiologic activity found with SPECT/CT, many MRIs or CTs may not help identify the pain generator and are likely unnecessary. In contrast, SPECT/CT offers efficient identification of the pain generator, due to degenerative changes, ultimately reducing unnecessary imaging, invasive procedures, and potential risk caused by those procedures and surgeries.7,8,9
Another benefit of SPECT/CT is that other non-invasive treatments can be more precisely targeted. Many interventions, like manual manipulation and therapeutic exercise, may have better outcomes when specifically focused on areas of dysfunction. For example, if a patient is noted to have increased physiological activity at a lumbar disc level, the patient may benefit from lumbar extension-based exercise. Whereas, a patient with increased activity of a zygapophyseal joint may worsen with extension-based exercise.
Who can benefit from SPECT/CT?
The ideal patient for a SPECT/CT bone scan is a patient that presents with chronic and persistent pain or non-radiating pain that is localized to a body region and associated with loss of active range of motion. Typically, patients are over 40 years of age and often present with some degenerative changes on X-ray. The following four examples illustrate these factors and how SPECT/CT performed on a Symbia Intevo™ with xSPECT Bone™ aided my clinical decision-making process.
Case 1
A 48-year-old woman was referred for posterior midline neck pain of 8/10 on the visual analog scale (VAS), which radiated to the cape of both shoulders. Symptoms began after she fell face forward on ice, several weeks after a C5-6 anterior cervical discectomy and fusion (ACDF) two years prior. Symptoms were exacerbated by driving and working. However, the symptoms were temporarily relieved by twice weekly visits with a chiropractor. She denied numbness and tingling or any bowel or bladder dysfunction. Past medical history was relevant for a planned breast reduction the following month, to help alleviate neck pain.
Cervical range of motion (ROM) testing was limited by 25% in all planes with reproduction of right-sided neck, midline neck, or occipital pain. Her neurological exam was normal for motor, sensory, deep tendon reflexes (DTRs), and the absence of other upper motor neuron signs.
The patient was advised to begin physical therapy, stop chiropractic treatment, and obtain a cervical X-ray with flexion/extension views (Figure 1). Recommendations to perform a left C3-4 and C4-5 zygapophyseal joint (z-joint) injection and order a cervical SPECT/CT (Figure 2) were also given.
Her cervical X-ray showed a prior C5-6 ACDF with intact fusion hardware, but no effort-induced listhesis, and no fracture. Z-joint injections did not improve the patient’s symptoms.
The subsequent cervical SPECT/CT radiologist report showed intense activity across the C5-6 level where there is evidence of prior fusion (Figure 2). The activity may represent ongoing osteoblastic activity, which if present for an extended period of time, could represent non fusion with residual instability. A subsequent cervical CT demonstrated a persistent bony cleft at the C5-6 vertebral level, which correlated with intense uptake on the cervical SPECT/CT (Figure 3).
The patient was diagnosed with pain from a C5-6 pseudoarthrosis of a prior C5-6 ACDF. Her pain improved after a cervical interlaminar epidural steroid injection (ILESI) and administration of a cervical brace. Two months later, a second cervical ILESI brought her additional pain relief and she was referred to a new orthopedic surgeon, who performed an iliac crest bone graft ACDF of her C5-6 level.
Case 2
A 91-year-old male patient presented with midline, constant, and sore, neck pain (4/10 VAS) near the base of the cervical spine. Pain began 17 months prior, with no known injury or cause and was aggravated by mowing the lawn. He denied numbness, tingling, or any prior neck injury.
Cervical ROM testing was 50% limited with flexion and left or right rotation, 75% limited with extension, and 100% limited with left or right side bending. ROM testing in all planes reproduced left-sided neck pain. The neurological test had normal motor strength sensation, Babinski’s sign, and Hoffman’s sign. DTRs were normal, except for 0/4 for Achilles bilaterally.
Cervical X-ray with flexion/extension views, demonstrated lateral displacement of the dens towards the left C1 articular process (Figure 4 and Figure 5). A left C3-4 and C5-6 z-joint injection provided no benefit.
A cervical CT was ordered to better characterize the displaced dens, which demonstrated the following:
- 100% displacement of the dens to the left without posterior dislocation.
- Severe degenerative changes of C1-2 lateral facets, all intervertebral disc levels, and all zygapophyseal joints.
- Near-bony fusion of C3-4 and C4-5 z-joints and C5-6-disc level (Figure 6).
A subsequent cervical SPECT/CT showed intense activity across the articulation of the left side C1-2 lateral masses. The patient was diagnosed with neck pain due to C2 dens lateral dislocation with severe left C1-2 lateral facet arthritis. A left C1-2 facet injection was then performed, which relieved the patient’s pain. He continued to improve with physical therapy afterwards (Figure 7).
Case 3
A 46-year-old woman was referred for left-sided lower back pain (9/10 VAS), which began three years ago following a colon resection. Her pain was exacerbated with prolonged standing and walking but eased with sitting. Ten sessions of physical therapy gave short-lasting relief. She also complained of numbness and tingling in bilateral lower limbs. Past medical history was remarkable for prior tubal ligation, hernia repair, carpal tunnel surgery, hysterectomy, colon resection, prior insufficiency fractures of her right foot and ankle, mild COPD, sleep apnea, and alcoholism.
On exam, her lumbar ROM showed full flexion, 50% limited extension, and full bilateral side bending without radiating symptoms. Her neurological exam had normal motor testing, DTRs, and tone. However, pinprick sensation was decreased in a stocking glove distribution up to bilateral knees.
A lumbar MRI showed only mild degenerative changes and no evidence of stenosis or impingement (Figure 8). An electrodiagnostic study demonstrated acquired generalized sensory-motor polyneuropathy of mixed nature. The patient had no benefit with two left sacroiliac joint injections.
A SPECT/CT showed severe left L5-S1 facet activity. She was diagnosed with pain from left L5-S1 facet osteoarthritis and unrelated pain from peripheral polyneuropathy (Figure 9). Subsequently, she had great temporary relief with a left L5-S1 and L4-5 facet steroid injection but had a less robust response with a repeat injection six months later. She ultimately had great persistent relief with radiofrequency ablation (RFA) of the left medial branches of L3 and L4 and the left dorsal ramus of L5.
Case 4
A 64-year-old female was referred by podiatry for persistent inside sharp right foot incision pain (6/10 VAS) that radiated to her ankle bone, following decompression of the right tarsal tunnel. Movement and walking increased her symptoms. She denied any new numbness or tingling following surgery and differentiated this pain from her previously diagnosed peripheral neuropathy. Her past medical history was significant for long-standing peripheral polyneuropathy and low-back pain.
The physical exam showed decreased pinprick in stocking glove distribution up to distal 1/3 of her legs with intact joint position sense (JPS) and reflexes bilaterally. Motor testing was normal, except for 3/5 left abductor digiti quinti (ADQ) and 1/5 right ADQ.
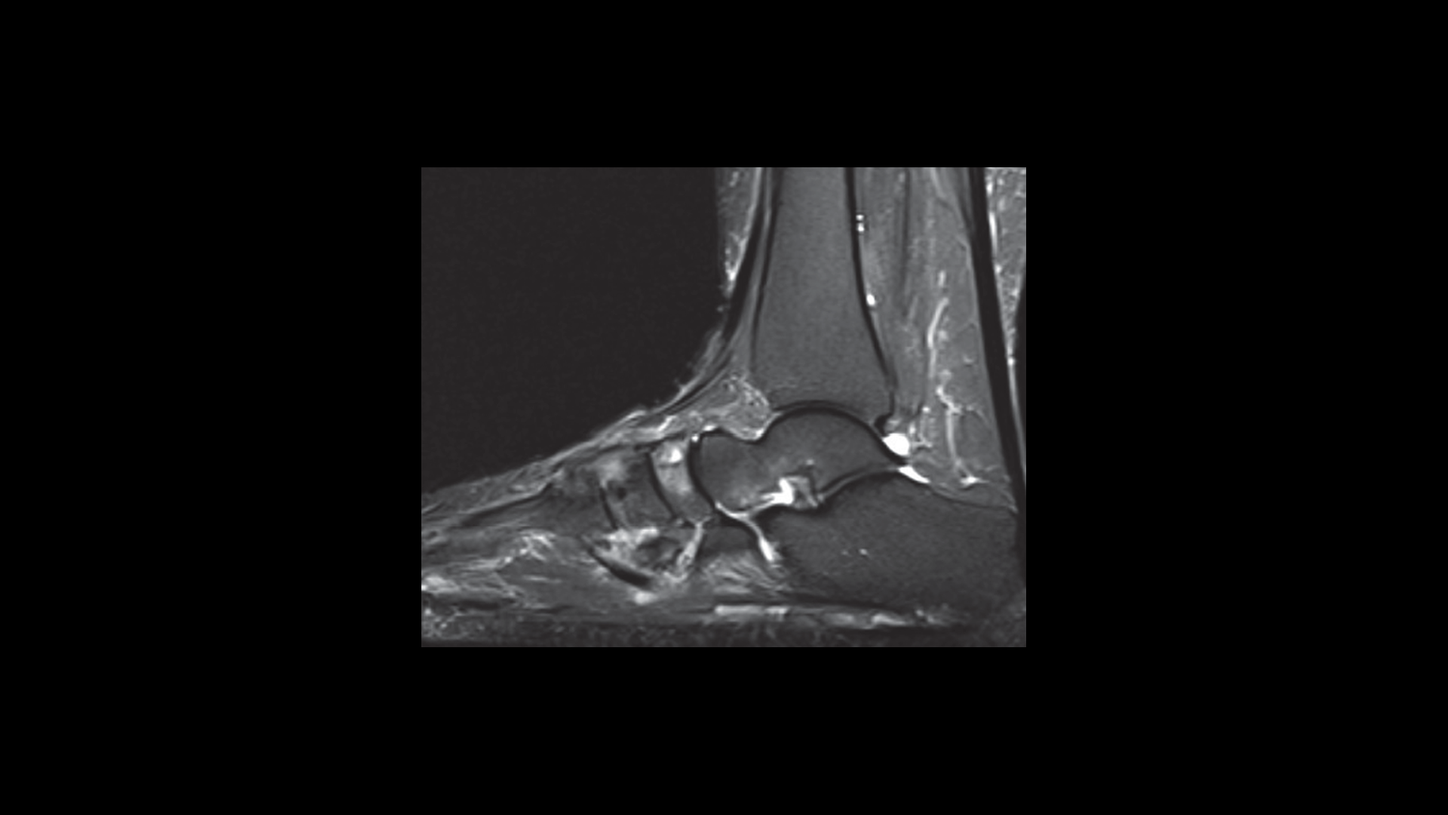
An MRI performed shortly before her tarsal tunnel decompression surgery showed:
- Moderate midfoot arthrosis involving the navicular cuneiform and third and fourth CMC joints with associated reactive marrow edema.
- Pes planus deformity of the hindfoot with diffuse fatty atrophy of the adductor digiti minimi muscle, correlate for Baxter’s neuropathy.
- No MRI scan evidence suggested plantar fasciitis (Figure 10).
A musculoskeletal ultrasound was performed which ultimately showed no evidence of entrapment of the tibial nerve by scar tissue. The patient failed to improve with a diagnostic steroid block of the medial plantar nerve of the tibial nerve.
A SPECT/CT image of the right foot was ordered, and the radiology report noted an intense accumulation within the right navicular and across the articulation of the navicular with the first cuneiform. The report identified a moderate accumulation within the lateral cuneiform, as well as across the articulation of the middle cuneiform and the lateral cuneiform. The report also described a mildly increased uptake in the base of the fourth metatarsal (Figure 11).
The patient was ultimately diagnosed with mechanical right foot pain due to midfoot degenerative joint disease and was counseled to follow up with Podiatry. Treatment options discussed included: orthotics, supportive shoes, non-steroidal anti-inflammatory drugs (NSAIDs), injections, and surgery to fuse the midfoot joint. Ultimately, the patient chose non-surgical treatment.
A key role in musculoskeletal care
SPECT/CT is a valuable imaging modality for the musculoskeletal physician and currently accounts for 20% of the advanced images that I order. SPECT/CT imaging will be of great interest to physicians to show Medicare and private insurance companies the ability to provide better care and potentially, lower healthcare costs. The Centers for Medicare and Medicaid Services (CMS) began value-based payments which moves away from paying providers based on the quantity of care they give patients, and toward lowering healthcare costs. This modality’s ability to efficiently improve identification of the pain generator in spine pain patients helps to reduce the risk of unnecessary imaging, invasive procedures and surgeries, and makes treatment more targeted and effective.10 These benefits align with not only the stated goals of CMS, but also the goals of all physicians. As more providers learn about this imaging modality, the utilization of SPECT/CT will likely increase and expand in the future of musculoskeletal care.
About the author
Dr. Ethan Colliver’s clinical practice is as varied as his clinical interests. In addition to being an expert at treating neck and low back pain, Dr. Colliver is one of few physicians in Southwest Virginia who treats chronic painful conditions such as chronic daily headaches, cervical dystonia, and spasticity with Botulinum Toxin (BOTOX) Injections. He was also the first physician to bring ultrasound-guided diagnosis and ultrasound-guided pain-relieving injections to the Blacksburg region. Dr. Colliver has expertise in reading musculoskeletal imaging such as MRIs and CT scans.