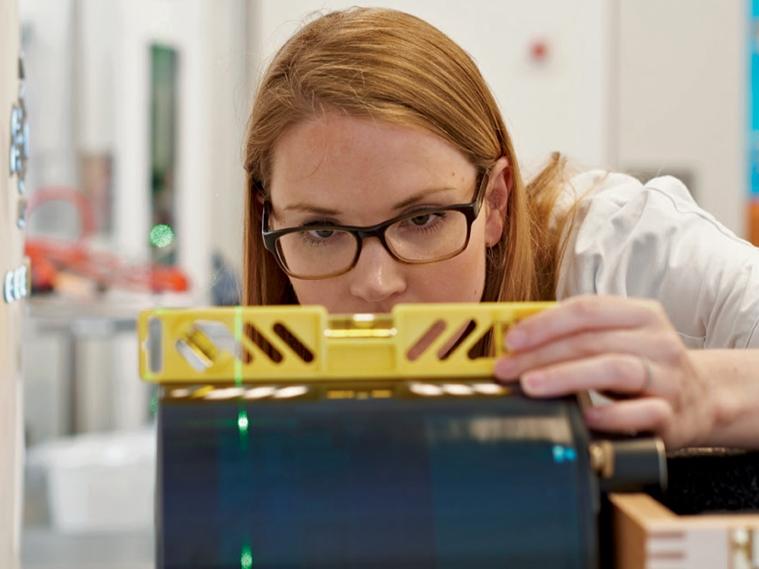
Today’s image-guided radiation therapy can be applied with great precision. One growing challenge is the increasing amount of metal in patients’ bodies, which leads to artifacts in CT images and obscures vital information. Laura Ann Rechner, Medical Physicist at the Rigshospitalet Department of Oncology, Section of Radiotherapy in Copenhagen, Denmark, is exploring how to solve this challenge using the iMAR algorithm.
Photos: Morten Koldby
Setting up a treatment plan for cancer patients with metal implants has so far required physicians to manually correct metal artifacts in the area of interest. Information about the tumor extension can be lost, and surrounding soft tissue needing protection from the radiation may remain undetected. In order to avoid the consequences of corrupted pictures, images must be manually corrected and contouring structures partially created using guesswork – this is a time-consuming and laborious task, and may result in inter-observer variability. In turn, this could jeopardize the levels of precision that today’s radiation therapy can achieve.
This challenge is becoming more of an issue as metal implants are on the rise in most countries. Almost all head and neck patients have metal in the form of dental fillings, which obscure parts of the CT images. In pelvis and spine tumor cases, the situation is similar since spinal and hip implants are becoming increasingly common.

“So far, we override such a region by calculating it as water or air as our best guess, knowing that this is not correct,” explains Rechner. “The precise contouring can be very time-consuming and difficult in these cases.” Up to now, there was no better way to deal with the effects of metal implants. None of the techniques currently proposed for metal artifact reduction are in widespread clinical use, as some add artifacts or remove valuable information. This is why Laura Ann Rechner began exploring the potential of the iMAR (iterative metal artifact reduction) algorithm last fall. She was able to address these critical issues in comparative studies with patient cases and phantoms.
Rechner tested the accuracy of iMAR in patient and phantom studies. One case that she found particularly convincing was that of a patient with cervical cancer who was treated with interstitial (MUPIT-type) pulsed dose rate (PDR) brachytherapy. “In this case, we lost a little information in the center due to the numerous metal implants, which resulted in somewhat blurred CT HUs (Hounsfield units) in the middle. But we decided that it was more useful to see the needles clearly,” Rechner explained. “This case convinced us to use iMAR as standard on all of our scanners in order to better serve our patients with metal implants.”
In her phantom study based on a tongue tumor, Rechner first performed contouring in the usual way. She then added the implant to the phantom and took the image with and without iMAR. Applying the algorithm, she was able to reduce the metal artifacts for a better image. The same was true for a pelvic phantom of a hip implant.
Reduction of streak artifacts

Another case with impressive results using iMAR involved a patient with a bladder tumor and two metal hip implants. For most patients with hip implants, the artifact would be an irritation that one would have to draw over in contouring, but in this case the target was very much affected by the artifact. On the regular image, there was no information on the key region of interest, making it difficult to decide where to treat. The algorithm helped to reduce the artifacts, according to Rechner.
She tested multiple iMAR algorithm reconstruction kernels, each relating to a different metal density, size, and degree of artifact, and making sure that the HU were all correct. After comparing the different delineations and dose calculations with the usual procedure when drawing in water, the dose was roughly equivalent.
According to Rechner, those patients scheduled for stereotactic radiation in particular may benefit. In these cases, small lesions need to be treated with a high degree of accuracy and with high doses, and therefore require images with reduced metal artifacts.
Fig. 1: In patients with metal implants, such as dental fillings (Fig. 1A), shoulder and hip implants (Fig. 1B), and pacemakers (Fig. 1C), using the metal artifact reduction algorithm iMAR (right column) can make it easier to reconstruct images accurately.
Great flexibility
Overall, iMAR reduces metal artifacts by combining three successful approaches: beam hardening correction in sinogram regions that have less severe metal attenuation; normalized sonogram inpainting in sinogram regions that have high metal attenuation; and frequency split to mix back noise texture and sharp details that are potentially lost during inpainting. The correction process is iteratively refined by repeating the normalized sinogram inpainting and the mixing steps up to six times. In turn, this leads to fewer artifacts, as an evaluation of artifact quantification using gold markers revealed. The risk of new artifacts is reduced thanks to Adaptive Sinogram Mixing, which flexibly combines normalized interpolation and a soft reduction metal artifact algorithm depending on the severity of the artifacts.
Radiologist Anne Kill Berthelsen, MD, works in the radiation therapy department and believes that iMAR has great potential. “We are pretty convinced that it will reduce metal artifacts – mainly from dental fillings or from hip implants – in gynecological tumors. This will be a big improvement, as we don’t know in advance which metal implants will lead to metal artifacts for which patients. We mostly hope to use it for head and neck patients where there are big holes in the scan. The radiation oncologists demand images with less and less metal artifacts as they want to make their radiation therapy more and more precise.”
Reconstruction with iMAR is fast. It takes one to two minutes with a choice of eight different reconstruction modes (neuro coils, dental fillings, spine implants, shoulder implants, pacemaker, thoracic coils, hip implants, extremity implants). Rechner recommends trying multiple types of reconstruction modes and devising the best strategy for each new type of metal implant.
"We are pretty convinced that iMAR will reduce metal artifacts. So radiation therapy can be provided more and more precisely."
Easy to use on all tailored scanners
At the Rigshospitalet of the University of Copenhagen – an institution with over 10,000 employees, more than 1,600 beds, and around 100,000 inpatients and 650,000 outpatients – about 70 doctors, 16 physicists, and 25 radiographers work at the Department of Oncology. Altogether, 500 employees take care of approximately 4,000 patients per year. Until now, iMAR has been running on a SOMATOM Definition AS Open – RT Pro edition. Soon it will be running on all scanners as standard.
Based on her experience so far, Rechner sees the application for iMAR mostly in head and neck patients, as well as for pelvic patients.
Rechner underscores the two main advantages of iMAR: Firstly, “iMAR saves us time, which we love.” Secondly, according to the medical physicist, “iMAR helps the patient, as the main objective of our treatment planning is to optimize the balance between efficiently treating the tumor and sparing the surrounding tissue. The reduction of metal artifacts that is possible with iMAR helps us do our job.”
She is curious about combining iMAR with 4D CT in patients with thoracic tumors and dental fillings. The team already tried combining Dual Energy CT and iMAR. When using 130 kV Dual Energy CT and iMAR, they were quite happy with the metal artifact reduction from iMAR alone. Since soft tissue contrast is presumed to be better at 70 kV, they now hope to achieve better metal artifact reduction together with better soft tissue contrast and lower energy.
"iMAR saves us time, by reducing metal artifacts."
With regard to the workflow, it is too soon to tell. “In the beginning, incorporating iMAR added a little time to the process, as we compared the image and HU values to our standard of care. But in the long run, it will save us time. Besides, patient outcome might be better, as we can target what we want to treat and protect, what we want to spare.”
About the Author
Wiebke Kathmann, PhD, is a frequent contributor to medical magazines. She holds a Master in Biology and a PhD in Theoretical Medicine and was employed as an editor for many years before becoming a freelancer in 1999. She is based in Munich, Germany.