Whole-body MRI (WB-MRI) is a hot topic – you may have had enquiries from colleagues asking you if or when you might be able to offer the service. You may not know where to start or what is involved. The purpose of this article and the accompanying video tutorial is to introduce and guide you through the implementation for successful completion of a MET-RADS compliant WB-MRI protocol [1].
WB-MRI has been used as a clinical tool at Paul Strickland Scanner Centre for over 10 years. In that time over 6,500 patients have been examined using a protocol designed to enable the detection and surveillance of metastatic bone and soft tissue disease. Treatment regimens are routinely being altered based on serial qualitative and quantitative measurements produced by this technique [2].
To enable the serial analysis of quantitative ADC measurements we must reduce acquisition variables as far as practicable. Clearly it is not possible to fully control all patient variables between visits. The patient’s condition may change, requiring a different coil set-up.
Adjusting scan parameters at a visit-by-visit basis adversely affects the reproducibility of both the qualitative and quantitative results. For the majority of sequences described below it is advised that the parameters are not adjusted by operators after initial protocol set-up. The sequences should be designed and saved to accommodate your largest (A>P and R>L) and tallest (H>F) patients by default, and ranges should not be reduced (e.g. phase FOV) even when this may normally prove advantageous. Those parameters which may be altered on a per-patient basis will be mentioned. Any changes made should remain constant between visits in the same patient where practicable.

Coil requirements
- Standard posterior spine coil
- Standard head & neck coil
- 2x anterior Body 18 coils as required for coverage to mid-thigh (3x recommended)
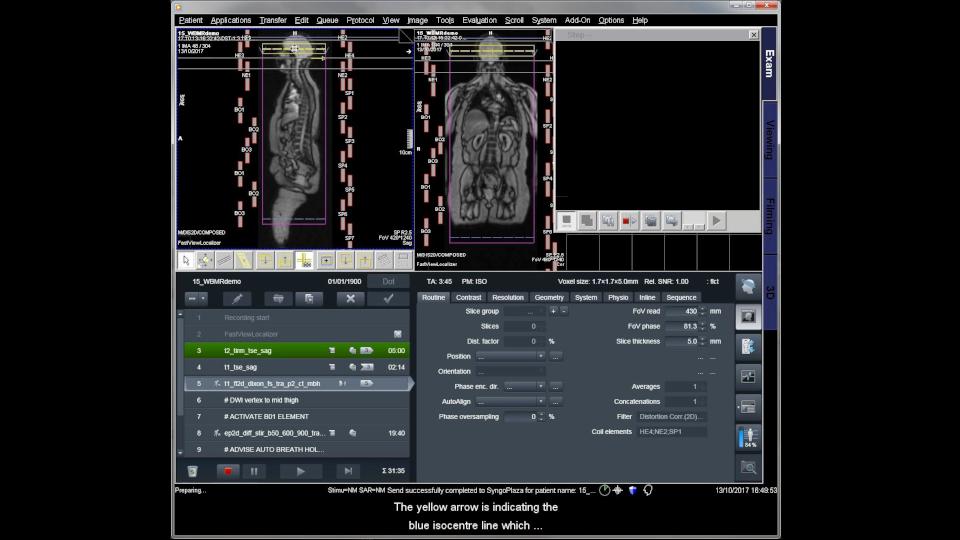
Number your Body coils and routinely positioning them in the same order will limit any sensitivity variability and also make coil troubleshooting much more straightforward. It is important to note that the range required for MET-RADS compliant protocols is from vertex to mid-thigh (Fig. 2). Although not always required, access to 3x Body 18 coils is optimal and should accommodate even the tallest patients.
As such it’s not necessary to use a peripheral coil for this protocol. If full imaging of the lower limbs is required it is advised to perform imaging separately and feet-first, allowing a bio-break for the patient.
As this technique will be used to generate quantitative ADC measurements it is especially important to ensure that the coils are working well. A coil QA program should be implemented with increased frequency of testing for the regularly used coils.
Patient comfort
Patient comfort is absolutely critical to compliance with this protocol, so utilize any equipment required for comfort (e.g. extra padding, pillows, knee pad, etc.). The patient should be advised to use the toilet where possible because the full protocol can take up to one hour. Patients will warm up – particularly when scanning at 3T – and so the patient should wear a gown or entirely metalfree light clothing. Ensure adequate air flow to reduce the impact of heating.
Find out if the patient is able to hold their breath – if they can, use a breath-hold technique when scanning the chest and abdomen to reduce motion artifacts.
Sequence selection
If you are using the downloadable .exar1 protocol you will find sequences which have been included and optimized based upon the experience of scanning around 30 whole body examinations each week.
You should expect the protocol to take anywhere between 30 to 60 minutes depending on what is included.
Please see the MET-RADS document [1] for the clinical justification of sequences included, however it may be helpful to touch briefly upon how the sequences have been optimized and how they can be used clinically.

The tricky part with WB-MRI is the initial set-up – don’t be surprised if your first efforts don’t produce the results you expect. A typical completed data set (Fig. 5) can consist of over 6,000 images depending on the sequences chosen and reconstructions performed, but once the protocol is in place it’s fairly straight-forward for operators to perform. In our experience, treating each examination as an experiment rather than a scan will lead to success. Keep up to date at www.siemens.com/wb-mri for the latest news, case studies and the video tutorial.
About the Author

Will McGuire is Deputy Superintendent Radiographer at Paul Strickland Scanner Centre in Northwood, Middlesex, UK
Whole-body MRI has been used as a clinical tool at Paul Strickland Scanner Centre for over 10 years. In that time they have performed over 6,500 examinations, using a protocol designed to enable the detection and surveillance of metastatic bone and soft tissue disease.