History
A 7-year-old girl was diagnosed in October 2016, with stage IV mediastinal neuroblastoma with osteomedullary bone infiltration. During the first year following diagnosis, the patient underwent different chemotherapy regimens and received treatment according to protocol NRNBL 1.7/SIOPEN (November 2016-January 2017) and TVD followed by TOTEM (February 2017-December 2017).
A follow-up MIBG scintigraphy (December 2017; images not shown) exhibited positive response to chemotherapy and displayed a decrease in the tracer uptake and number of bone lesions. However, there was persistent uptake in the left upper thoracic-paravertebral mass.
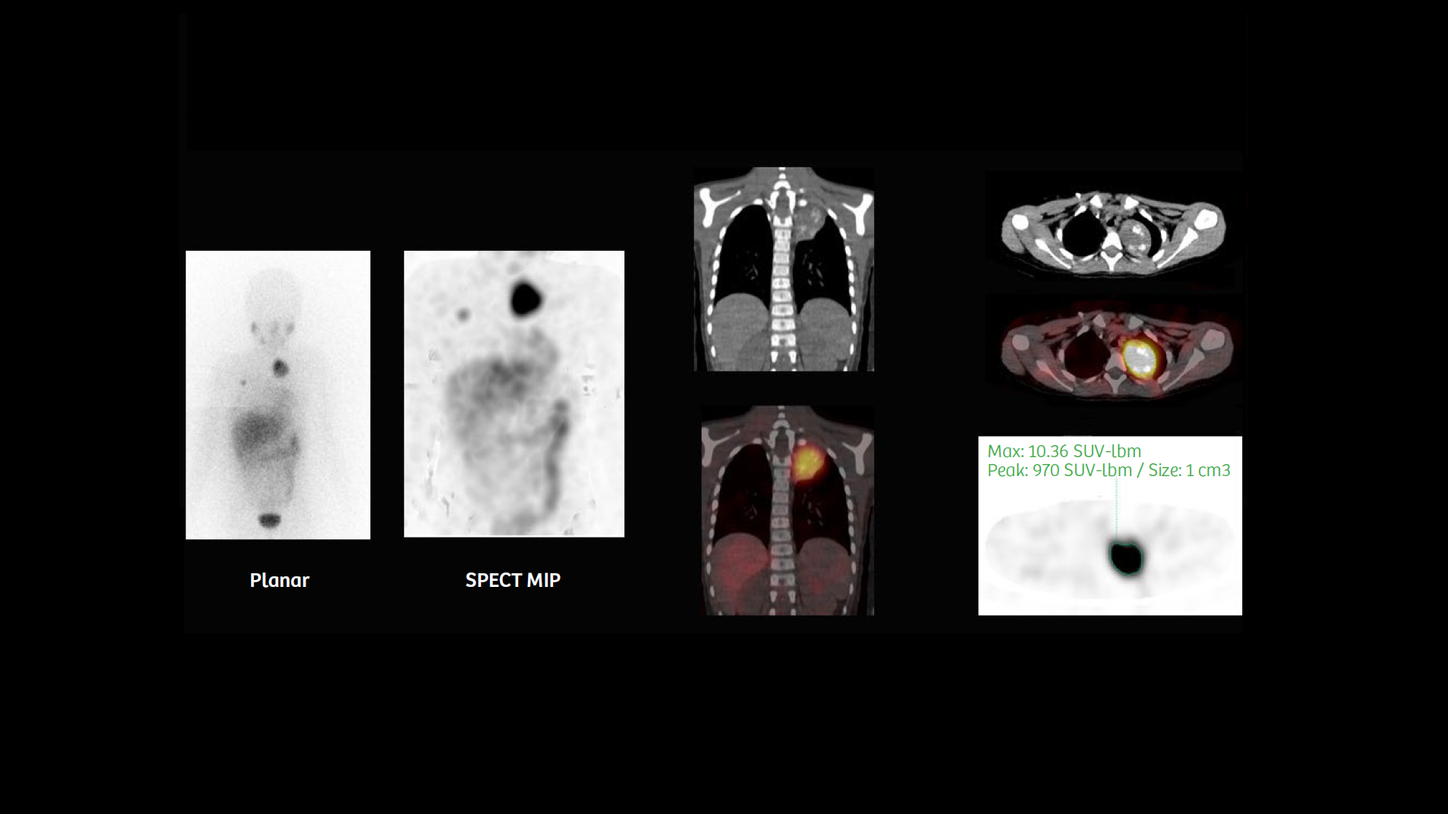
Subsequent treatment included the administration of 6.9 GBq of Iodine-131 (131I) MIBG (January 2018-February 2018), followed by stem cell reinfusion (February 2018). A follow-up Iodine-123 (123I) MIBG scintigraphy was performed in March 2018, with SPECT/CT using a Symbia IntevoTM with xSPECT Quant™ (the first xSPECT acquisition) for absolute quantification of 123I MIBG uptake. An intravenous injection of 111.6 MBq of 123I MIBG (patient weight 48.5 lb/22 kg) was administered for a whole-body planar and SPECT/CT acquisition of the thorax and abdomen, performed 24 hours post injection. An initial CT was performed (80 kV, 30 eff mAs, 16 x 1.2 mm collimation), followed by a SPECT acquisition at 30 stops with 30 seconds per stop; the study was reconstructed with xSPECT Quant.
Findings
Compared to the initial 123I MIBG scintigraphy (December 2017), the followup 123I MIBG SPECT/CT (March 2018)— performed one month after 6.9 GBq 131I MIBG therapy—showed decreased uptake in the 5th rib bone lesion and stable uptake in the mediastinal lesion, without any new bone uptake on visual assessment. The SUVmax values obtained from the xSPECT Quant study provided a quantitative benchmark for subsequent evaluation of the MIBG-avid thoracic lesion.
The patient underwent a new cycle of high-dose chemotherapy with Busilvex®/melphalan (April 2018), followed by autologous stem-cell reinfusion that same month.
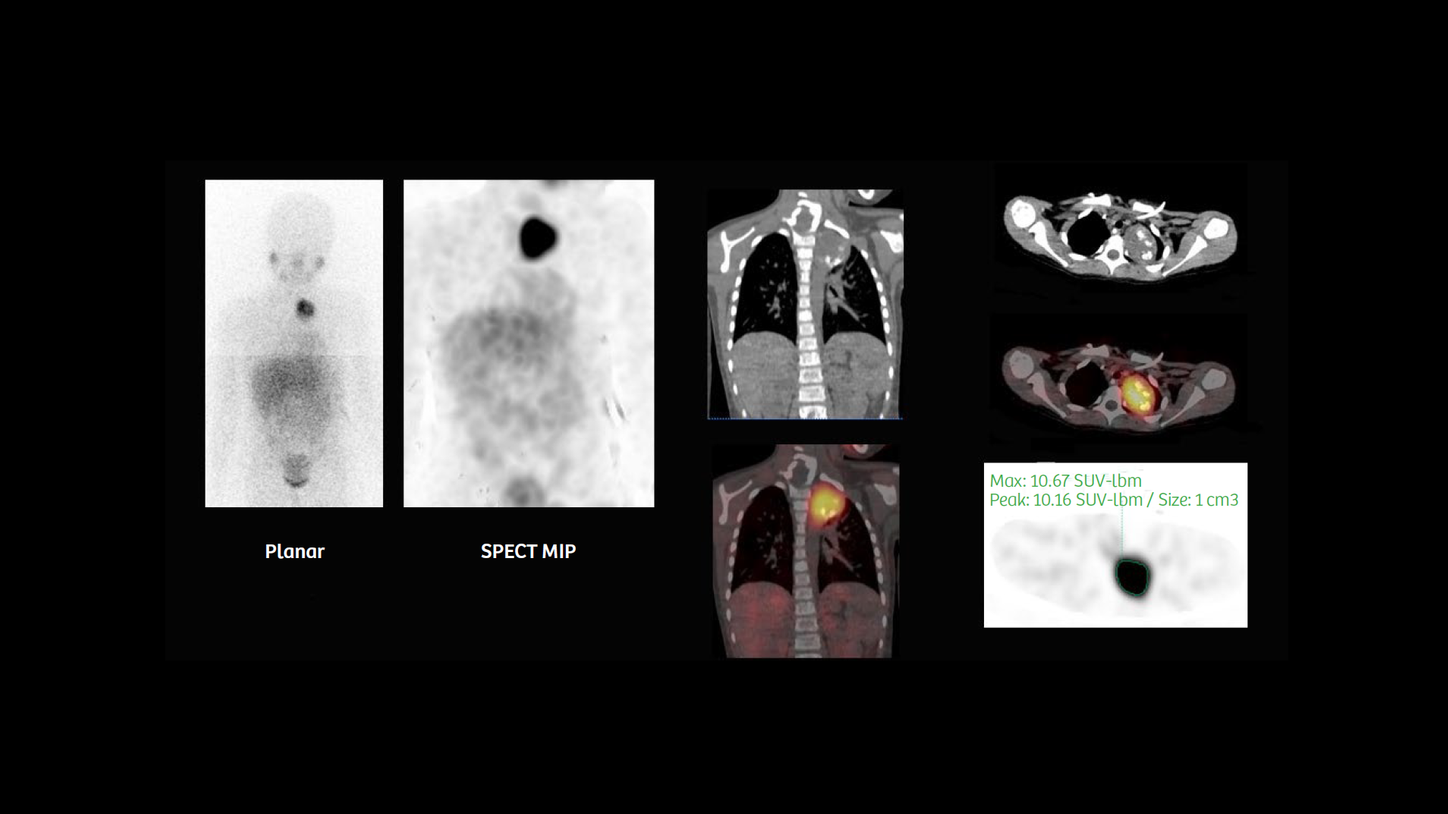
A follow-up 123I MIBG SPECT/CT study with xSPECT Quant was performed in May 2018, (the second xSPECT acquisition) using a similar injected dose with the same acquisition parameters as the initial xSPECT Quant study.
As noted in Figure 2, the second followup 123I MIBG SPECT/CT study showed mediastinal lesion stability based on both visual and quantitative assessment (SUVmax: 10.67 versus 10.36 g/ml). In the absence of progression, the patient underwent surgical resection of the left superior mediastinal tumoral mass (June 2018). Post-surgery thoracoabdominal MRI (July 2018) showed no residual lesion in the resection site, which was filled by a loculated pleural effusion. A follow-up 123I MIBG SPECT/CT study (August 2018, the third xSPECT acquisition) confirmed the absence of tracer uptake in the resection site with minimal postoperative remodeling. No new suspicious lesions were detected on the whole-body images.
Comments
In this case, the visual impression between the sequential 123I MIBG SPECT/CT studies performed in March 2018 and May 2018 suggested an absence of any significant change in tumor size and intensity of uptake. However, the SUVmax values provided quantitative confirmation of the stable nature of the mediastinal lesion, which did not decrease in size or uptake intensity despite the high-dose 131I MIBG therapy and additional chemotherapy. In view of the absence of new metastases and the relatively stable volume and functioning tumor burden of the mediastinal lesion, which was quantitatively evaluated by sequential xSPECT Quant, the decision for surgical removal of the tumor was adopted. Post-surgery scintigraphy shows positive results with a complete removal of the functioning tumor mass and an absence of new metastases as well as postoperative fibrosis.
Conclusion
This case demonstrates the value of xSPECT Quant to act as a precise and objective tool for evaluating neuroblastoma patients—allowing for the assessment of tumoral activity on baseline MIBG scintigraphy, chemotherapy, or metabolic radiotherapy response, as well as remission after surgical treatment. Accurate knowledge of tracer uptake can guide a successful therapeutic plan by helping establish an appropriate treatment modality dependent on tumoral-activity evolution.
Examination protocol
Scanner: Symbia Intevo