History
A 13 year old female patient, presented at the emergency department complaining of acute left lower abdominal pain and vomiting. She was referred to the radiology department with a clinical suspicion of renal/ureteric calculus. Whole abdomen low dose non-contrast CT was performed for detection of urinary system calculus. The KUB CT showed a centrally located large cyst in the pelvis with uterus deviated to the left. Ultrasound and MRI performed for further evaluation.
Diagnosis
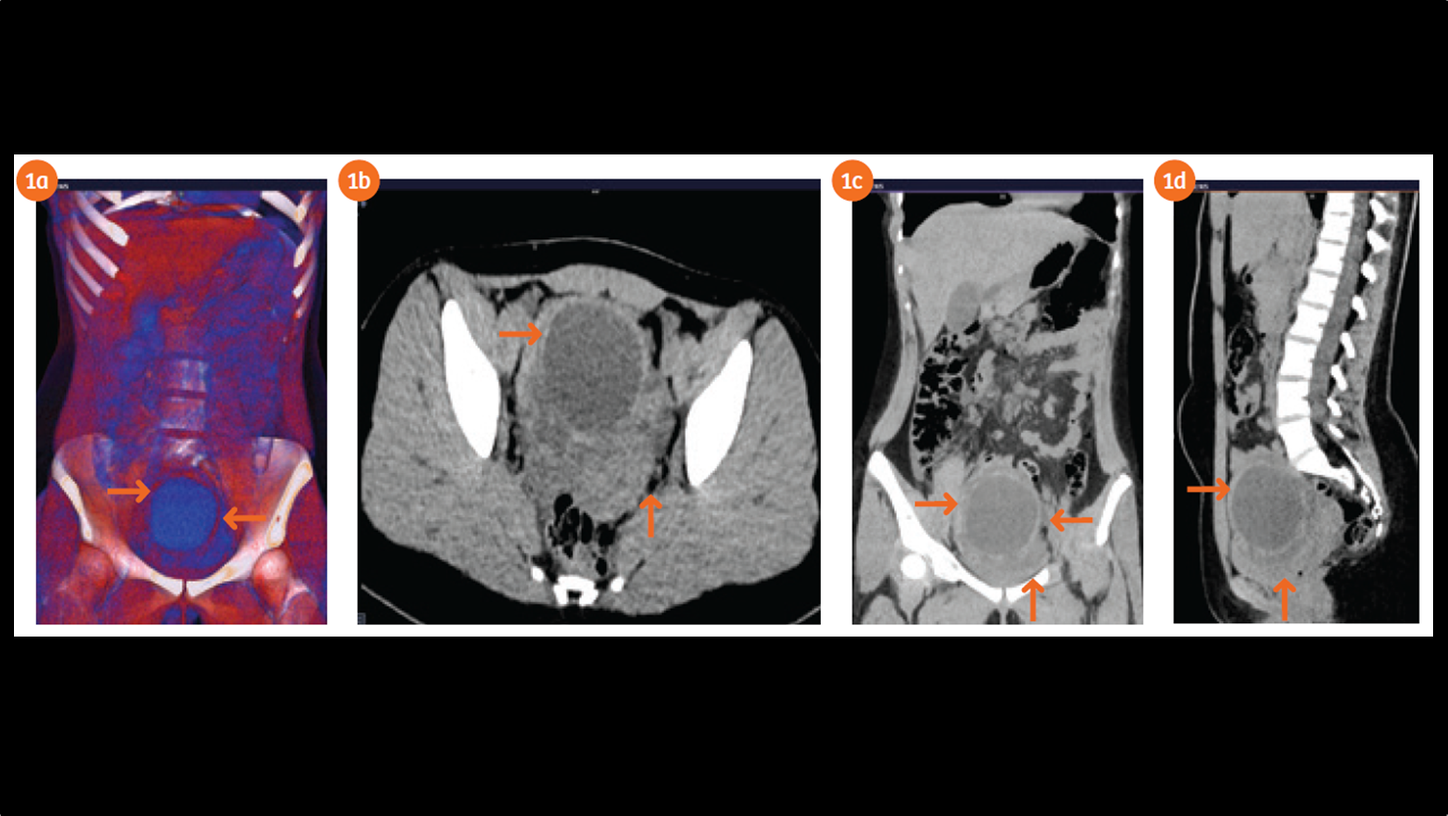
Whole abdomen low dose CT (ctdivol 160 mGy.cm and effective dose 2.4mSv) performed on SOMATOM Flash 256 slices machine showed a left-sided pelvic large cystic lesion measuring 7 x 8 cm in diameter (Figs. 1a–1d). There is no evidence of abnormal calcification within or in the wall of the cystic lesion. The lesion is causing significant mass effect on the urinary bladder and uterus. No renal stone is seen. No ureteric or pelvi-calyceal dilatation seen particularly in the left side. The rest of the structural anatomy includes kidneys, gall bladder, upper and lower abdominal areas appear to be normal.
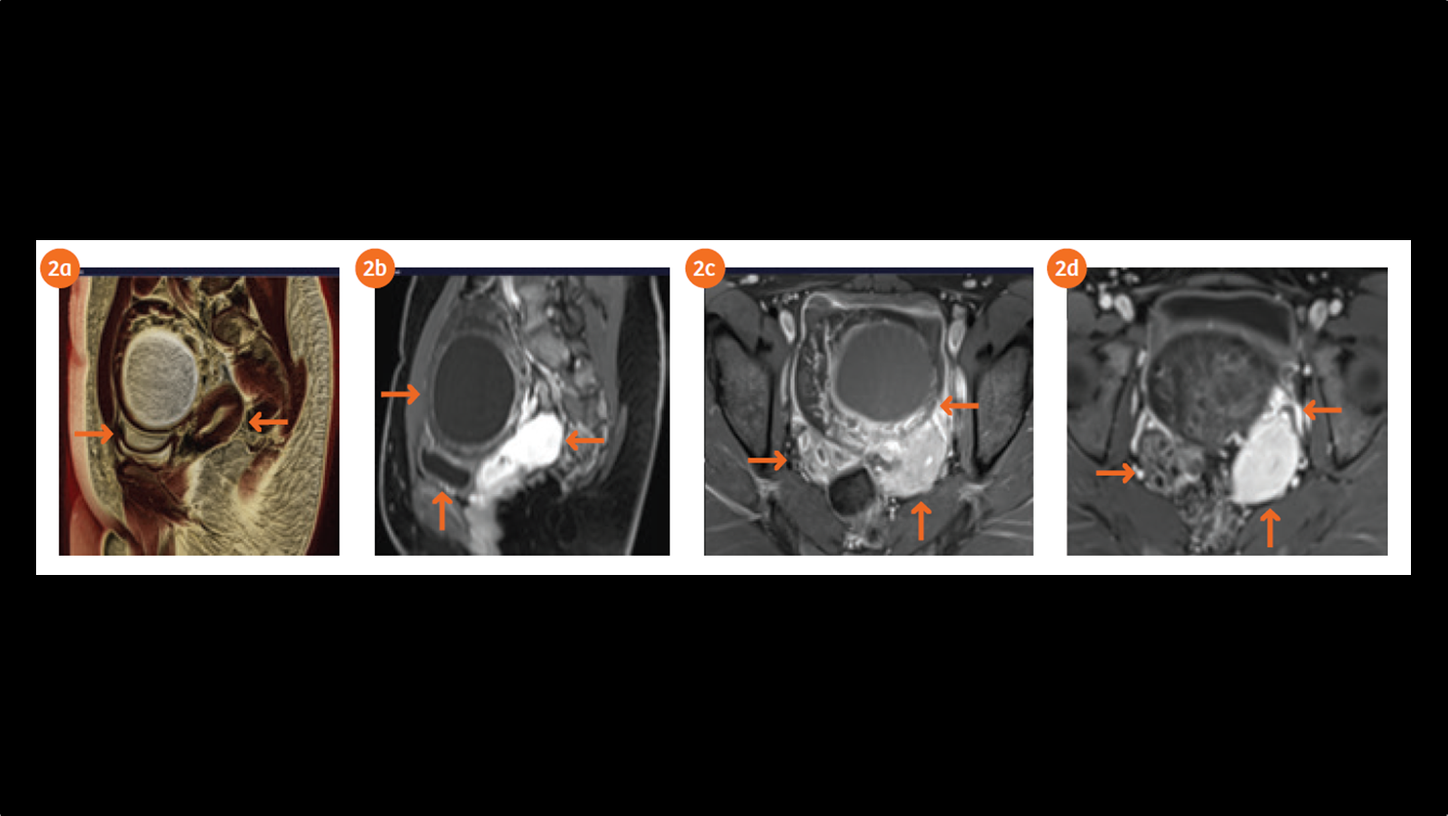
The pelvic ultrasound showed significant enlargement of the left ovary exhibiting a large anechoic cyst with edema of the ovarian stroma and free intraperitoneal fluid effusion. The color Doppler showed persistent arterial vascularity in the left ovary. The US appearance of the ovary raised high suspicion of left ovarian torsion. The pelvic MR exam performed on MAGNETOM Skyra 3T system demonstrates a large rounded hemorrhagic cyst within the left ovary measuring 70 x 70 mm in diameter with regularly thickened wall causing compression of the urinary bladder and displacing posteriorly the uterine body. The high tissue characterization MRI revealed edema and multiple foci of hemorrhage in the left ovarian stroma with twisting of the vascular pedicle in the left adnexa. Patient underwent surgical procedure and that lead to the torsion correction and cyst removal. After three months in the follow up ultrasound evidence, both the ovaries and the uterus were normal.
Comments
Most patients with ovarian cysts are asymptomatic but large ovarian cysts are a common source of acute pelvic pain. Among women with ovarian disorders, ultrasound is the primary imaging modality for the evaluation of pelvic pain in women in child bearing age. However, Computed Tomography (CT) is the frequently requested radiology exam in non-pregnant patients who present to emergency departments with nonspecific abdominal and pelvic pain.
CT particularly with low dose capability has several advantages the exam can be performed immediately and can be easily accessible (24x7). Furthermore, CT of the abdomen or pelvis allows broad evaluation of all abdominal and pelvis structures. Unenhanced KUB CT scan is preferably requested for patient presenting with renal colic symptoms. Low dose CT technique like SAFIRE, CARE DOSE 4D and low CARE kV imaging make sure that the delivered dose will be as low as possible. The illustrated study is a proven example for low dose with a total delivery of 2.4 mSv with high diagnostic value.
Magnetic resonance imaging is being used more frequently for problem solving. The MRI exam allows a comprehensive ovarian and other pelvic structure evaluation for pre surgical planning, particularly if there is a high degree of concern of ovarian torsion persists. Diffusion weighted imaging and gadolinium-enhanced fat-saturated breath-hold pulse sequences play a crucial role in improving the specificity of MR value in diagnosis of ovarian torsion. Given the large differential diagnosis of acute non pregnant women pelvic pain, a structured approach of multi-modality image interpretation is invaluable.
Examination Protocol
Contact:
The outcomes by Siemens Healthineers customers described herein are based in results that were achieved in the customer’s unique setting. Since there is no ”typical” hospital and many variables exist (e.g. Hospital size, case mix, level of IT adoption), there can be no guarantee that other customers will achieve the same results.
References
1. Guthrie BD, Adler MD, Powell EC. Incidence and trends of pediatric ovarian torsion hospitalizations in the United States, 2000-2006. Pediatrics 2010;125:532-8. Epub 2010 Feb 1.
2. Z. Tsafrir, J. Hasson, I. Levin, E. Solomon, J.B. Lessing, F. AzemAdnexal torsion: cystectomy and ovarian fixation are equally important in preventing recurrence Eur J Obstet Gynecol Reprod Biol, 162 (2) (2012), pp. 203-205
3. Oltmann SC, Fischer A, Barber R, Huang R, Hicks B, Garcia N. Cannot exclude torsion - a 15-year review. J. Pediatr. Surg. 2009;44:1212-6; discussion 1217.
4. Aziz D, Davis V, Allen L, Langer J. Ovarian torsion in children: Is oophorectomy necessary? J. Pediatr. Surg. 2004;39:750-3.
5. Servaes S, Zurakowski D, Laufer MR, Feins N, Chow JS. Sonographic findings of ovarian torsion in children. Pediatr. Radiol. 2007;37:446-51. Epub 2007 Mar 15.
6. Cass DL. Ovarian torsion (review). Semin. Pediatr. Surg. 2005;14:86-92.
7. Beaunoyer M, Chapdelaine J, Bouchard S, Ouimet A. Asynchronous bilateral ovarian torsion. J. Pediatr. Surg. 2004.
8. Oltmann SC, Fischer A, Barber R, Huang R, Hicks B, Garcia N. Pediatric ovarian malignancy presenting as ovarian torsion: incidence and relevance. J. Pediatr. Surg. 2010.
9. Huang TY, Lau BH, Lin LW, Wang TL, Chong CF, Chen CC. Ovarian cyst torsion in a toddler. Am. J. Emerg. Med. 2009;27:632, e1-3.
10. Houry D, Abbott JT. Ovarian torsion: a fifteen-year review. Ann. Emerg. Med. 2001.
11. Conforti A, Giorlandino C, Bagolan P. Fetal ovarian cysts management and ovarian prognosis: a report of 82 cases. J. Pediatr. Surg. 2009.
12. Meyer JS, Harmon CM, Harty MP, Markowitz RI, Hubbard AM, Bellah RD. Ovarian torsion: clinical and imaging presentation in children. J. Pediatr. Surg. 1995.