A critical component of many brain surgeries is mapping the cortical regions that are essential for language in order to maximally preserve these regions during surgery. However, pre-surgical language mapping tests are not available for many of the world’s languages, including Arabic as spoken in the UAE. Consequently, Arabic-speaking patients may be tested in a language that is not their native language or not tested at all. This can compromise the ability to localize core language areas, which may consequently lead to language deficits after surgery, especially in patients with tumors or epileptic foci near language cortex.
This work takes advantage of the advanced multi-modal neuroimaging and language expertise at New York University Abu Dhabi (NYUAD) to address both the need for basic neurobiological research on Arabic and the need for an Arabic language pre-surgical mapping protocol. The NYUAD team is collaborating with Cleveland Clinic Abu Dhabi (CCAD) to develop an Arabic mapping protocol based on a well-established protocol in English (Black et al., 2017, Am J Neuroradiol).
An effective language mapping protocol must cover all stages of language processing. In broad terms, for comprehension, this involves the perception of speech sounds or orthography, the mapping of word forms onto word meanings and the construction of complex syntactic and semantic representations. Production, in contrast, involves the construction of a message to be conveyed, mapping of that message to a syntactic structure, identification of the relevant lexical material, activation of the sound representations of those words, and finally motor planning of articulation.
In conclusion, utilizing advanced multi-modal MRI techniques including advanced structural segmentations, Arabic language mapping with fMRI, and diffusion tractography provide valuable tools for presurgical mapping of specialized cortical areas of language, which reduces intraoperative time to identify language centers in Arabic-speaking patients. On the other hand, the use of intraoperative direct electrical stimulation helps in validating the “correlative” data provided by fMRI-based language mapping, which can be helpful in the cases of tumor resections in fully anesthetized patients.

Fig 2: This patient went for an awake tumor resection surgery. The craniotomy location and corresponding contours (red trace) on the brain surface. Intraoperative electrical stimulation was performed to identify the eloquent language areas in close proximity to the tumor. Initially, a monopolar electrode was used to deliver electrical current intraoperatively during awake language tasks which caused speech arrest in the same locations that were identified from the Arabic fMRI (white and red dots on the pars triangularis area). During resection, continuous monopolar stimulation was used in the depth of the tumor to recognize subcortical connectivity of different language areas.
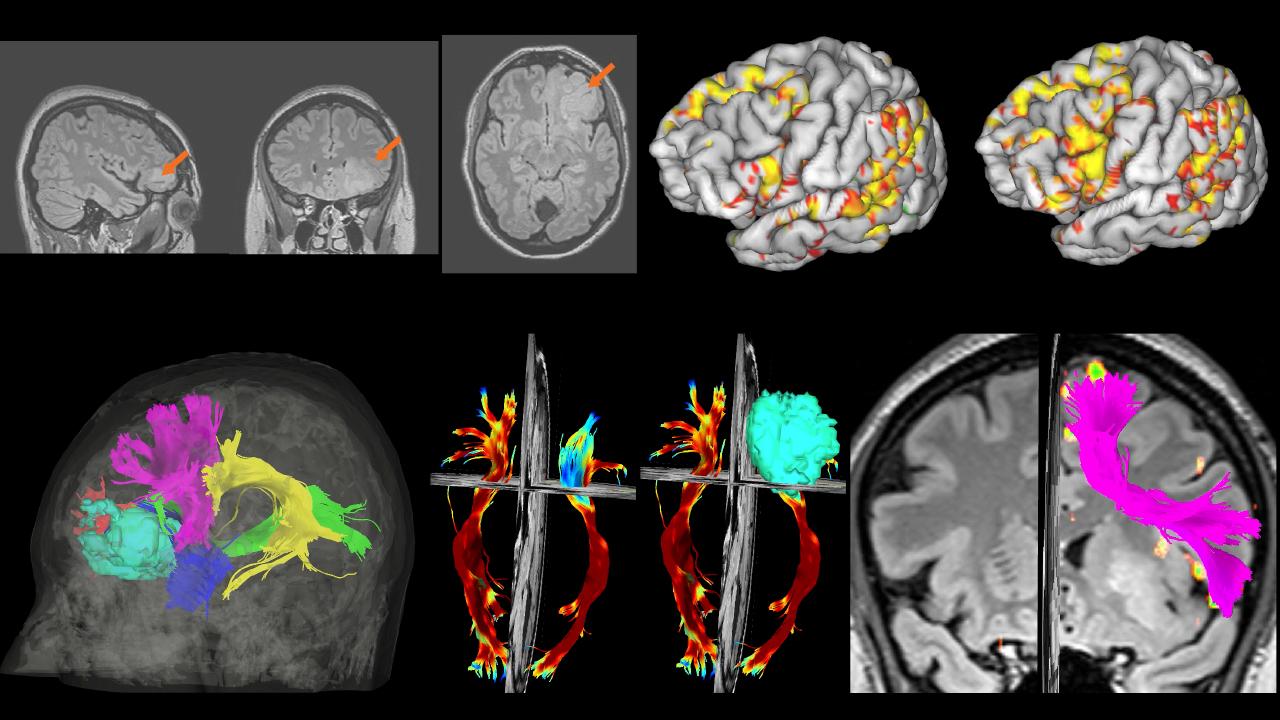
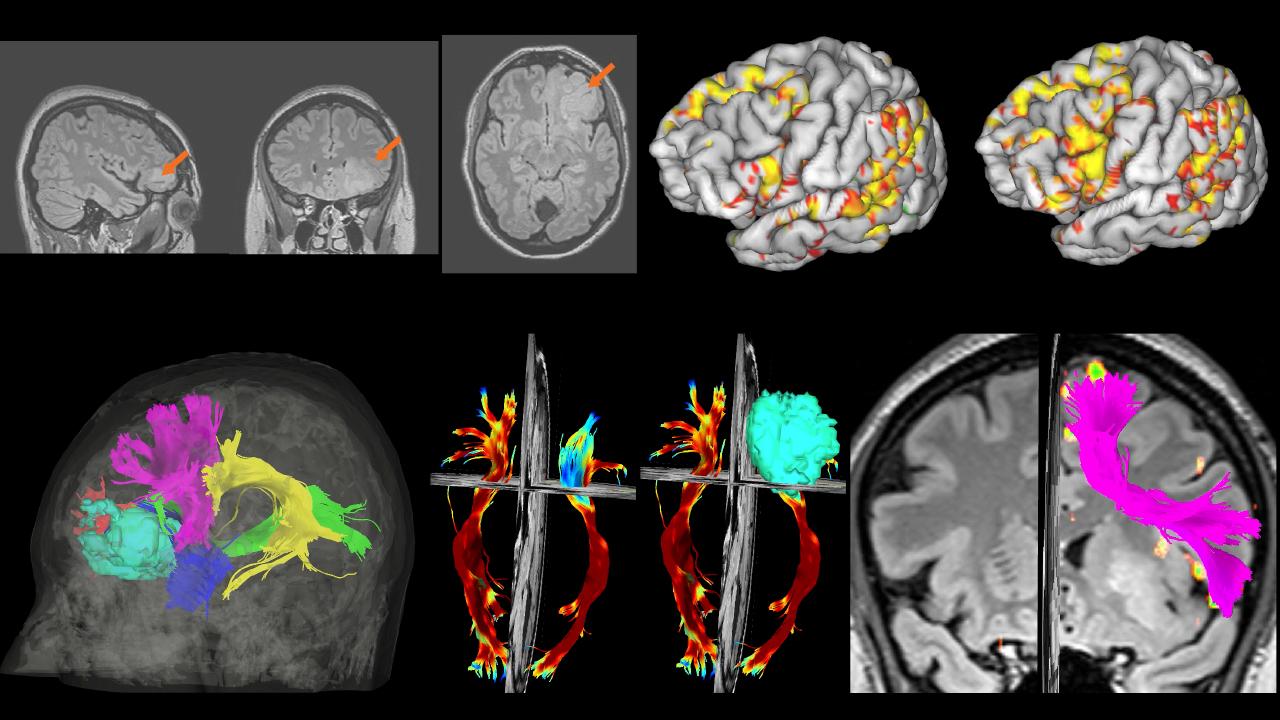
Fig 1: T2-FLAIR images of a patient with low grade glioma in the orbitofrontal area (white arrows). This patient performed 7 functional (fMRI) tasks in Arabic, only 2 tasks are shown (auditory questions, and a visual sentence completion task). The hot colors denote activations in the main language areas such as the pars triangularis/orbitalis, the posterior superior temporal gyrus, and dorsal and ventral premotor cortexes. Fiber tractography was also used to map the structural connectome and identify the white matter bundles that are critical for language. Shown in Fig. 1 fiber tractography overlaid on the tumor model (light blue), the arcuate fasciculus (yellow), the inferior fronto-occipital fasciculus (green), and the frontal aslant tract (purple).

Fig 2: This patient went for an awake tumor resection surgery. The craniotomy location and corresponding contours (red trace) on the brain surface. Intraoperative electrical stimulation was performed to identify the eloquent language areas in close proximity to the tumor. Initially, a monopolar electrode was used to deliver electrical current intraoperatively during awake language tasks which caused speech arrest in the same locations that were identified from the Arabic fMRI (white and red dots on the pars triangularis area). During resection, continuous monopolar stimulation was used in the depth of the tumor to recognize subcortical connectivity of different language areas.
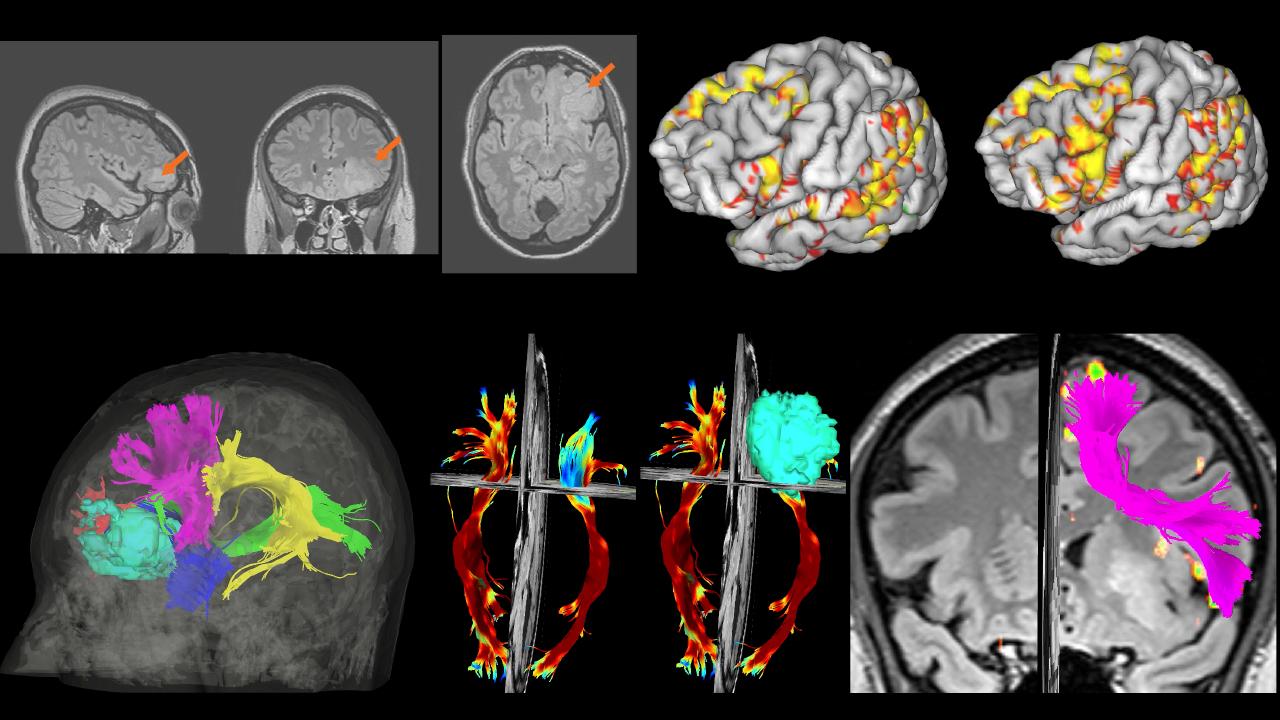
Fig 1: T2-FLAIR images of a patient with low grade glioma in the orbitofrontal area (white arrows). This patient performed 7 functional (fMRI) tasks in Arabic, only 2 tasks are shown (auditory questions, and a visual sentence completion task). The hot colors denote activations in the main language areas such as the pars triangularis/orbitalis, the posterior superior temporal gyrus, and dorsal and ventral premotor cortexes. Fiber tractography was also used to map the structural connectome and identify the white matter bundles that are critical for language. Shown in Fig. 1 fiber tractography overlaid on the tumor model (light blue), the arcuate fasciculus (yellow), the inferior fronto-occipital fasciculus (green), and the frontal aslant tract (purple).

Fig 2: This patient went for an awake tumor resection surgery. The craniotomy location and corresponding contours (red trace) on the brain surface. Intraoperative electrical stimulation was performed to identify the eloquent language areas in close proximity to the tumor. Initially, a monopolar electrode was used to deliver electrical current intraoperatively during awake language tasks which caused speech arrest in the same locations that were identified from the Arabic fMRI (white and red dots on the pars triangularis area). During resection, continuous monopolar stimulation was used in the depth of the tumor to recognize subcortical connectivity of different language areas.


Caregiver team at CCAD

The Neuroscience of Language Lab at NYU
Contact

Osama Abdullah
New York University Abu Dhabi and Cleveland Clinic Abu Dhabi