Addressing the rising prevalence of Non-alcoholic Fatty Liver Disease
Learn more about NAFLD, a leading cause of liver related mortality
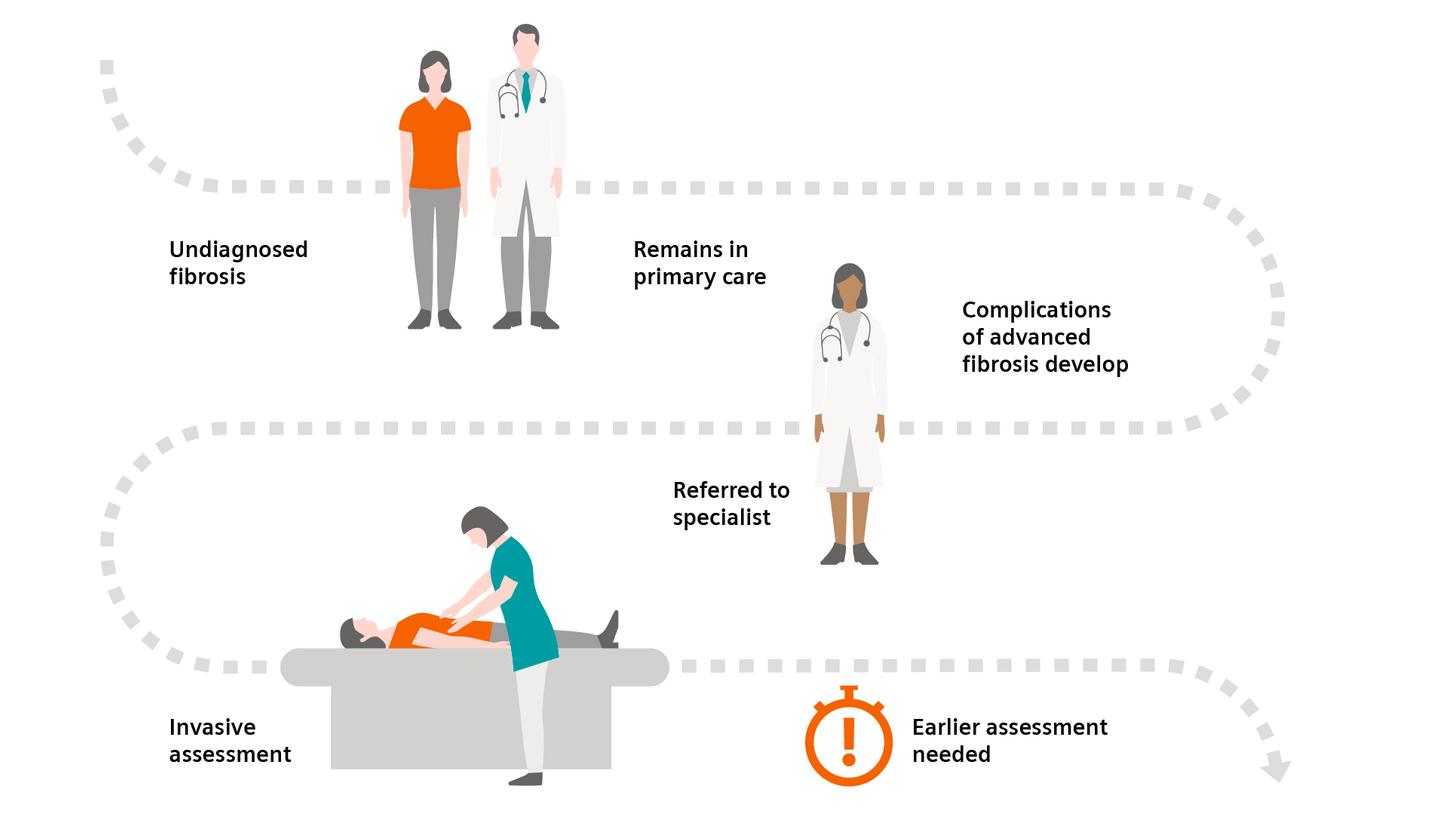
Non-alcoholic fatty liver disease (NAFLD) is a condition in which excess fat, not caused by heavy alcohol use, is stored in the liver. There are two types of NAFLD: simple fatty liver (simple steatosis) and non-alcoholic steatohepatitis (NASH).
The products/features (mentioned herein) are not commercially available in all countries. Their future availability cannot be guaranteed.
Younossi ZM, et al. Hepatology. 2016;64:73–84.
Pais R, Barritt AS 4th, Calmus Y, et al. J Hepatol. 016;65(6):1245–1257. doi:10.1016/j.jhep.2016.07.033.
Younossi ZM, et al. Diagnostic modalities for nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, and associated fibrosis. Hepatology. 2018 Jul;68(1):349-60.
Anstee QM, et al. Noninvasive tests accurately identify advanced fibrosis due to NASH: baseline data from the STELLAR trials. Hepatology. 2019 Nov;70(5):1521-30.