History
A 3-year-old female patient, complaining of dyspnea upon exertion as well as intermittent chest pain, was presented to the hospital. An echocardiography examination revealed a continuous flow in the lateral wall of the right ventricular outflow tract (RVOT), suspicious of a coronary-cavitary fistula, without describing the origin and the course of the fistula. A minimal degree of pulmonary regurgitation was also visualized, but all cardiac functional measurements were normal. A cardiac CT angiography (CTA) was requested for further assessment prior to treatment.
Diagnosis
CTA images showed a tortuous coronary fistula, originating from the proximal third of the left anterior descending artery (LAD) with a small caliber of 2 mm, coursing posteriorly, forming a network, encasing and finally draining into the left anterior wall of the main pulmonary artery (MPA), just distal to the pulmonary valve. The caliber and the course of the distal LAD were normal. Neither dilation in the proximal LAD and the MPA, nor signs of other accompanying anomalies were noted. A diagnosis of a single, isolated coronary arteriovenous fistula (Sakakibara type A) was suggested. The patient underwent surgical treatment. The postoperative evolution was satisfactory, without complications. She was discharged from the hospital on the fifth postoperative day. At a three-month follow-up, she was asymptomatic and had no alterations in the electrocardiogram.
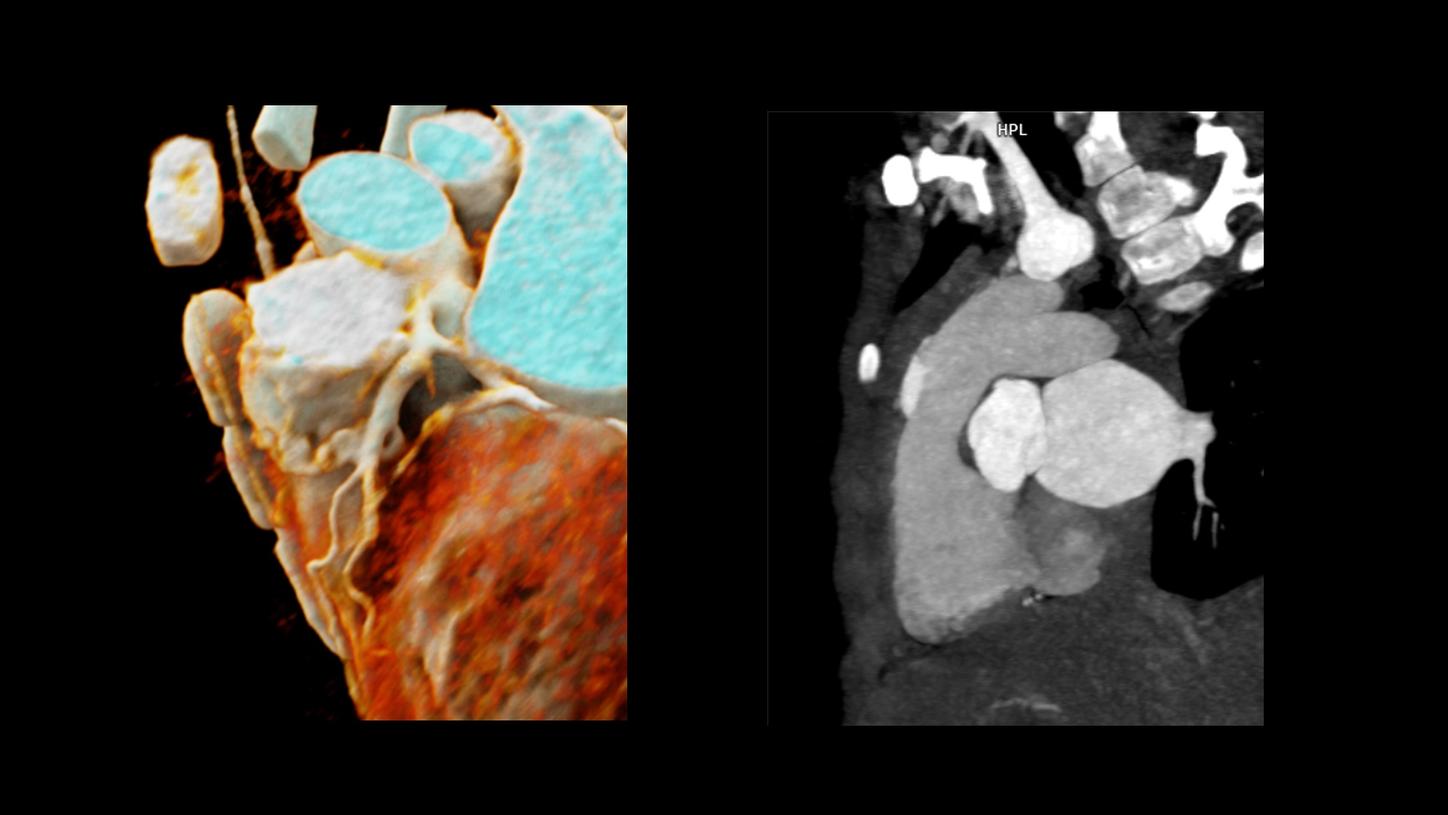
Fig. 1: A cVRT image (Fig. 1a), a MPR image (Fig. 1b) and a MIP image (Fig. 1c) show a single, small coronary fistula (Fig. 1a & 1c, arrows) originating off the proximal LAD, coursing posteriorly and draining into the left anterior wall of the MPA (asterisks), just distal to the pulmonary valve (Fig. 1b).
Comments
Congenital coronary artery fistulas (CAFs) may involve cardiac cavities as well as vascular structures. Variable clinical courses may occur, from asymptomatic to serious, e.g., with ischemic symptoms due to coronary flow steal, pulmonary hypertension and/or heart failure due to volume overload. The conclusive treatment of a CAF is to close its fistulous tract, either surgically or with a percutaneous procedure. It is essential for therapeutic planning to acquire detailed anatomical imaging information including the origin, the course and the drainage site of a CAF, as well as any associated anomalies. Echocardiography can be complimentary in providing cardiac functional information, however, there are difficulties in precisely visualizing the anatomical details of the fistula, such as in this case. Cardiac CTA has become an essential imaging assessment for the complex anatomy of CAFs. In combination with cinematic volume rendering technique (cVRT), lifelike images can be demonstrated in three dimensions facilitating an easy understanding and communication. One of the challenges in pediatric cardiac CT scanning is acquiring images without motion artifacts, as this group of patients usually has higher heart rates and breathhold difficulties. To overcome this, a high temporal resolution and an ultra-fast acquisition speed are mandatory. This case was performed with a dual source CT scanner, SOMATOM Force, which provides a temporal resolution of 66 ms as well as a “Turbo Flash” scan mode with ECG triggering and an acquisition speed of 737 mm/s. Although the patient had a heart rate of 146 bpm and was scanned at free breathing, the fistula between the proximal LAD and the MPA was clearly visualized with optimal image quality. Turbo Flash is an invaluable scan mode for pediatric patients allowing for the comfort of free breathing as well as ultra-fast scanning speed, contributing to a reduction in radiation exposure and the amount of contrast agent needed. This makes a so-called dual Turbo Flash mode – two Turbo Flash scans performed back-to-back – outstanding to ensure an optimal acquisition. This mode was successfully performed in this case, catching an ideal phase when there is no contrast agent in the right cardiac chamber and the pulmonary arteries, which would otherwise interfere with the visualization of the fistula.
Examination Protocol