History
A 42-year-old female patient (BMI 32.4), suffering from fever (37.8º C) and a moderate dry cough for the past week, presented herself to the hospital. She was a non-smoker and had an unremarkable past medical history. The RT-PCR test for COVID-19 resulted positive and she was then referred for a chest CT examination.
Diagnosis
CT images revealed multiple ground-glass opacities (GGO), with partial consolidation, affecting multiple lobes in both lungs. The lesions’ distribution was predominantly subpleural, posterior and peripheral, however bilateral central involvement was also seen. Additional findings such as septal thickening, pleural thickening, bronchial wall thickening, air bronchogram and bronchus distortion were also visualized. There were no signs of adenopathy or similar processes. The aorta and pulmonary arteries were unremarkable. Considering all clinical and epidemiological data, CT findings were consistent with the diagnosis of COVID-19 pneumonia.
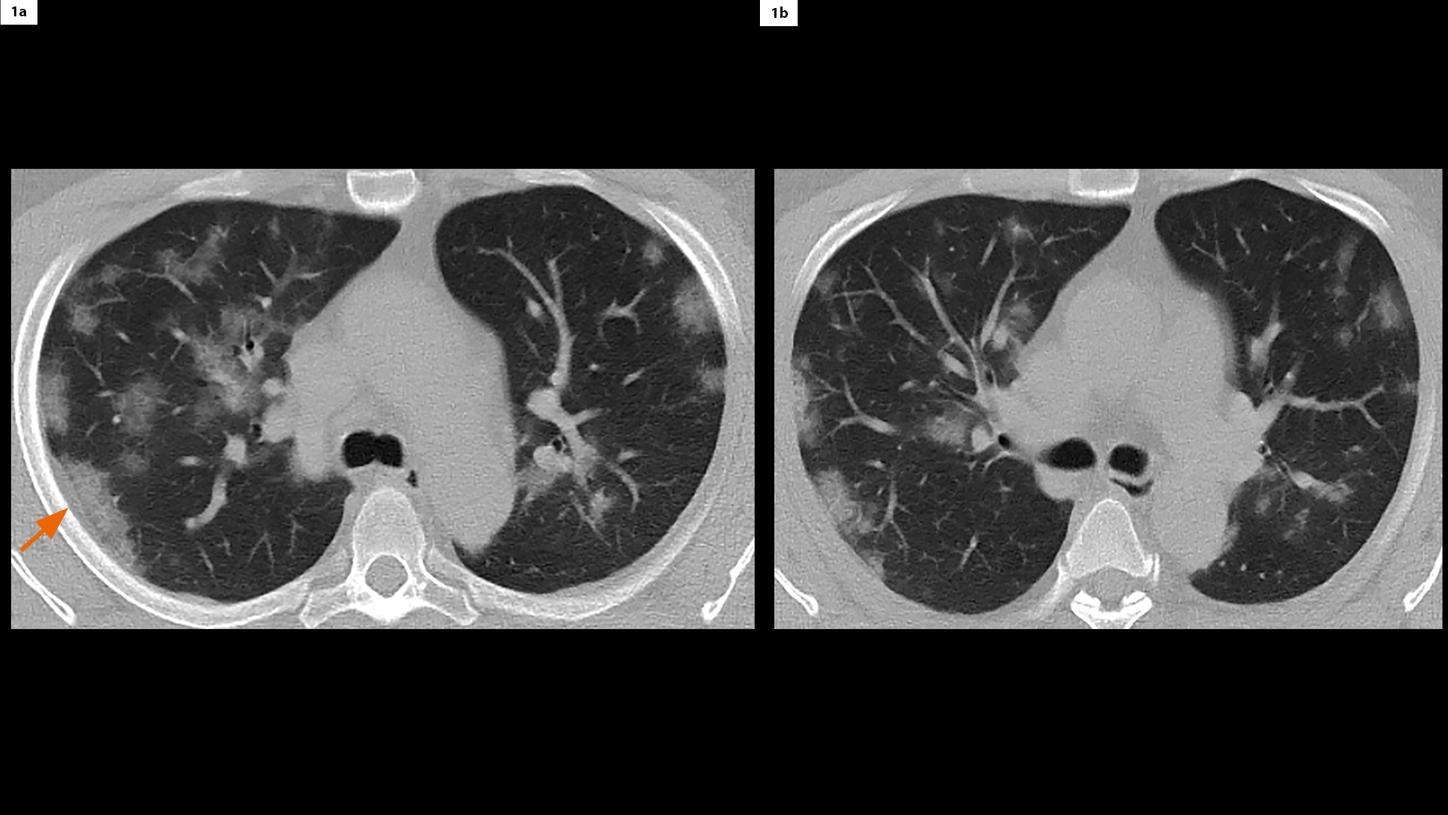
Fig. 1:
Axial images (4 mm) show both peripheral and central distribution of patchy GGO bilaterally in the lungs. Pleural thickening is also seen (Fig. 1a, arrow).
Comments
COVID-19 pneumonia is a viral infectious disease caused by a novel coronavirus (SARS-CoV-2). It is highly contagious, leading to a wide involvement of the global population and is currently a World Health Organization (WHO) declared pandemic. A chest CT examination is performed to assist diagnosis and assess complications. The primary CT findings include GGO and/or air space consolidation that can be bilateral, peripheral or basal in distribution. Image noise is usually well-tolerated when visualizing such patchy lesions in the lungs. Therefore, scanning with a lower radiation dose has great potential. In this case, we performed the CT scan with a low dose protocol using SOMATOM go.Now. The exposure reduction is enabled by an advanced tin filter technology, which optimizes the X-ray spectra and significantly improves the air / tissue contrast. The achieved image quality is considered to be optimal for diagnosis. This protocol should also be considered for follow-up scans. The acquired images can be reconstructed in multiplanar reconstruction (MPR), and volume rendering technique (VRT) to enhance the visualization of the lesions.
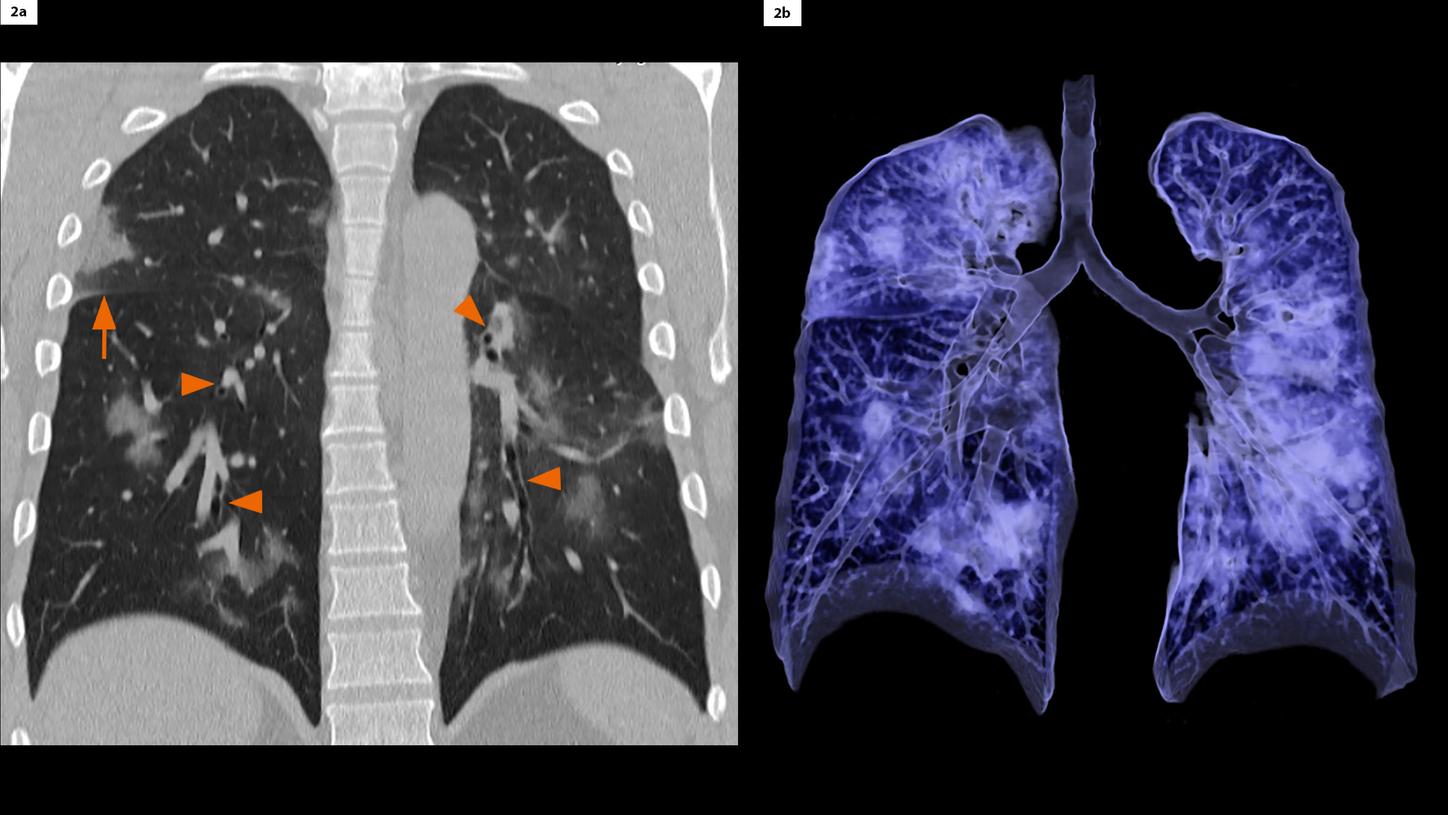
Fig. 2:
A coronal MPR image (Fig. 2a, 3 mm) and a VRT image (Fig. 2b) show multiple GGO in all lobes of both lungs. Signs of bronchial wall thickening (Fig. 2a, arrowheads) and septal thickening (Fig. 2a, arrow) of the right horizontal fissure are clearly seen.
Fig. 3:
A sagittal MPR image of the right lung (Fig. 3a, 2 mm) shows air bronchogram (arrow) and bronchus distortion (arrowhead) in patchy GGO with partial consolidation in the superior lobe. A sagittal MPR image of the left lung (Fig. 3b, 2 mm) shows multiple vacuoles inside patchy GGO in the inferior lobe (circle).