Home
Perspectives
- The MRI at 50 – what lies ahead?

The MRI at 50 – what lies ahead?
Magnetic resonance imaging (MRI) is the gold standard of imaging diagnostics in many medical fields. But it is still far from always being readily available – even where it would be the best option. Technological progress is rapid. The next generation MRI could look very different.
MRI today: The soft tissue giant

Key investigation areas for MRI are soft tissue areas like brain, abdomen, vessels, ligaments, cartilages or muscles.
Fig.1: Courtesy of Tongji Hospital, Wuhan, China

Key investigation areas for MRI are soft tissue areas like brain, abdomen, vessels, ligaments, cartilages or muscles.
Fig.2: Courtesy of Siemens Healthcare GmbH, Germany

Key investigation areas for MRI are soft tissue areas like brain, abdomen, vessels, ligaments, cartilages or muscles.
Fig3: Courtesy of Radiologische Gemeinschaftspraxis, Halle/Saale, Germany

Key investigation areas for MRI are soft tissue areas like brain, abdomen, vessels, ligaments, cartilages or muscles.
Fig.4: Courtesy of Clinique De L'infirmerie Protestante De Lyon, Lyon, France
The challenge of accessibility
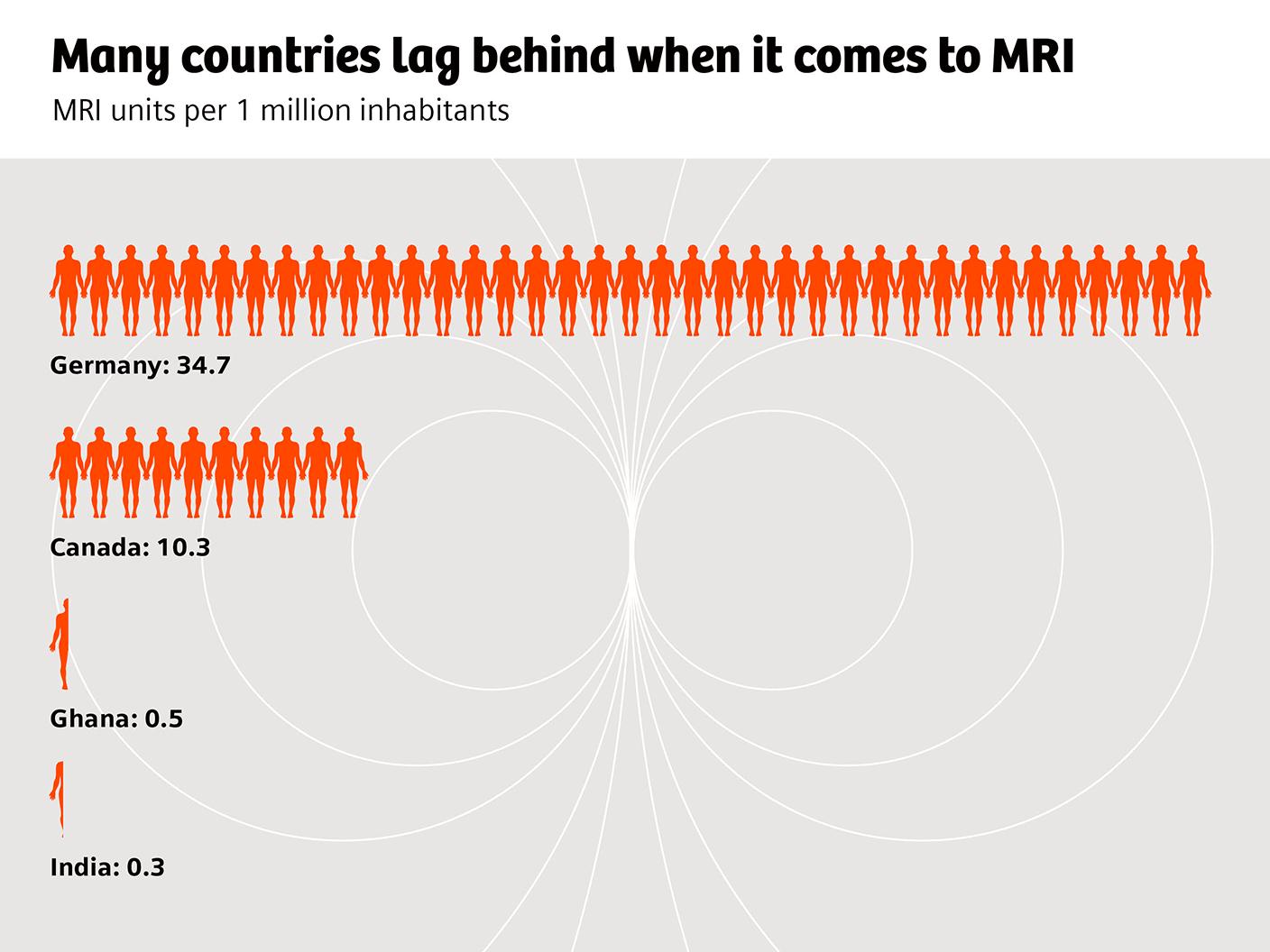
Despite its strengths, MRI is far from being universally accessible. In the OECD countries, for example, on average more than twice as many CT examinations as MRI scans are performed per 1000 inhabitants. Waiting times for an MRI scan are usually much longer than for a CT. There are also huge geographic variations: in Germany and Austria, the annual number of MRI examinations is bigger than the number of CT scans. In most other OECD countries, it is the other way round, and in less developed countries, the density of MRI scanning units is generally very low.
Other challenges

Some patients are too obese for MRI examinations, some patients have to be excluded if they suffer from claustrophobia.

Some patients are too obese for MRI examinations, some patients have to be excluded if they suffer from claustrophobia.
All in all, performing an MRI examination takes longer, and can be trickier than performing a CT examination. As a consequence, delegating an MRI examination to a technical assistant is less straight-forward than delegating a CT examination. Hub-and-spoke scenarios, increasingly common in CT imaging, are rare in MRI.
The transforming power of innovation
Enter the future of MRI diagnostics
Share this page
Philipp Grätzel von Grätz lives and works as a freelance medical journalist in Berlin. His specialties are digitalization, technology, and cardiovascular therapy.
The statements by Siemens Healthineers customers described herein are based on results that were achieved in the customer’s unique setting. Since there is no “typical” hospital and many variables exist (e.g., hospital size, case mix, level of IT adoption) there can be no guarantee that other customers will achieve the same results.











