Selective Internal Radiation Therapy (SIRT) is a relatively new procedure in interventional oncology. It offers great promise in the therapy of nonresectable hepatocellular carcinoma as well as colorectal, neuroendocrine, or breast cancer liver metastasis.
Application of SIRT
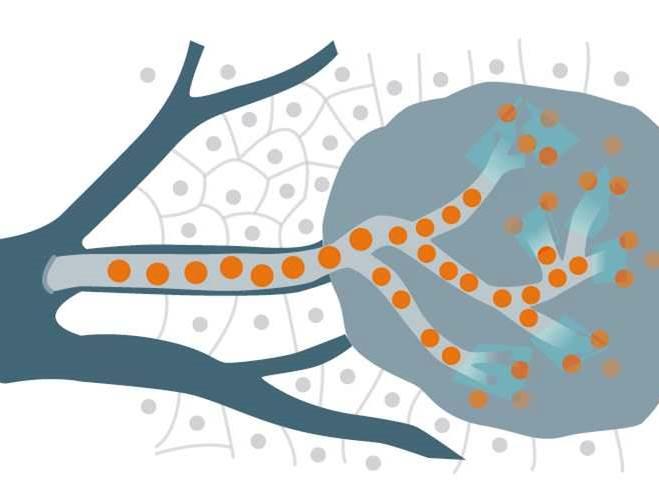
In these types of liver tumors local liver ablation techniques are of interest as external beam radiation is not an option in most cases due to the poor radiation tolerance of liver tissue. Serious or even fatal radiation hepatitis may result. By selectively delivering radiation dose directly to the tumor, SIRT treatment reduces systemic toxicity while optimizing treatment efficiency. SIRT cancer treatment works through the delivery of yttrium-90 microspheres to the tumor via the hepatic artery. This image-guided transcatheter tumor therapy, also known as transarterial radioembolization (TARE), can either be applied alone or in combination with transarterial chemoembolization or systemic chemotherapy respectively. Hence, it is suitable even for patients with high tumor load. It is not a cure but increases survival time and quality of life. In cases with intensive liver involvement tumor size may be reduced, thereby even opening up the possibility of secondary resection of hepatic tumors.

Goals of the pre-examinations during the work-up
- Exclude tumor manifestations outside the liver, evaluate tumor perfusion, and determine tumor distribution and load as well as liver volume with native or contrast enhanced computed tomography (CT) or magnetic resonance imaging (MRI) of chest and abdomen
- Exclude shunts between liver and lung by performing a scintigram
- Precisely determine the liver’s vascular anatomy with digital subtraction angiography (DSA) and cone beam CT

Angiography is key
SIRT cancer treatment normally consists of two steps – the preparation or work-up and the delivery of a single application of yttrium-90 microspheres into the hepatic artery:
Step 1: SIRT preparation:
- Assess hepatic arterial vasculature by 2D DSA imaging to obtain information of the tumor feeding vessels
- Prevent potential non-targeted embolization by occluding extra-hepatic vessels branching off the hepatic artery
- Ensure complete occlusion of aberrant vessels by performing cone beam CT
- Perform SPECT scan after intraarterial test-injection of 99mTc albumin particles (MAA) to determine the extent of arteriovenous shunting to the lungs and to confirm the absence of gastric and duodenal flow
- Assess patient's suitability for treatment and calculate the appropriate activity of radiospheres to be administered by considering liver volume, tumor volume and shunt fraction
Step 2: SIRT treatment:
- Position trans-femoral catheter at the predetermined treatment position with image-guidance based on the angiographic mapping
- Perform cone beam CT to prevent spill over into other gastrointestinal organs via aberrant vessels or newly developed vessels or anastomosis
- Deliver yttrium-90 microspheres into the microvasculature of the tumor while limiting the impact on healthy tissue

Siemens angiography and advanced applications provide an excellent support during SIRT procedures:
- Artis family offers complete portfolio of interventional angiography systems including floor-, ceiling-mounted, biplane system and the highly-flexible robotic system Artis zeego, allowing greater positioning flexibility and easy patient access
- Variety of planning and guidance tools such es syngo Embolization Guidance or syngo 3D Roadmap
- Intraprocedural 3D CT-like images with syngo DynaCT from head- left- or right-patient side make procedures safer and technically easier
- Understanding of the whole extent of the surrounding vessel anatomy with the extended volume provided by syngo DynaCT 360 on the Artis zeego angiography modality
- Evaluation of tumor blood volume information with syngo DynaPBV Body
- Utilize additional imaging information from CT, MR or PET-CT during your intervention with syngo Fusion package

