
Radiofrequency ablation (RFA) is a well-established procedure in the treatment of small solid tumors, mainly of the liver be it heptocellular carcinoma (HCC) or colorectal metastases. There is also a growing field of application in pain management, e.g. in bone metastasis. The high-energy radio wave treatment is applied in a needle-based approach under image-guidance (Ultrasound, CT, MRI or angiography).
Radio ablation treatment can be performed percutaneously, laparoscopically, or in open-surgery approaches. It can also be applied as an alternative to surgery or in addition to surgery, chemotherapy, embolization, or radiation therapy.
Application of RFA
It is an established therapeutical alternative in patients with few or small tumors (usually less than 2 cm in diameter) who are not eligible for surgery. In most cases radiofrequency ablation therapy is used for complete ablation of the tumor. Less often, it is performed as a bridging therapy in patients on the waiting list for a liver transplant for HCC treatment or as a strategy for de-bulking the tumor burden. For successful ablation, detailed knowledge about tumor extent, its proximity to larger vessels and surrounding tissue is essential.
To ensure a sustained treatment effect a complete ablation with a sufficient safety margin is crucial. As a thermal ablation procedure, RFA cancer treatment has the benefit of not causing widespread toxicity. It is therefore a chosen approach for recurring interventions (e.g. for local recurrence after RFA or tumor load control of the liver). Depending on tumor size and location several electrode insertions may be necessary.
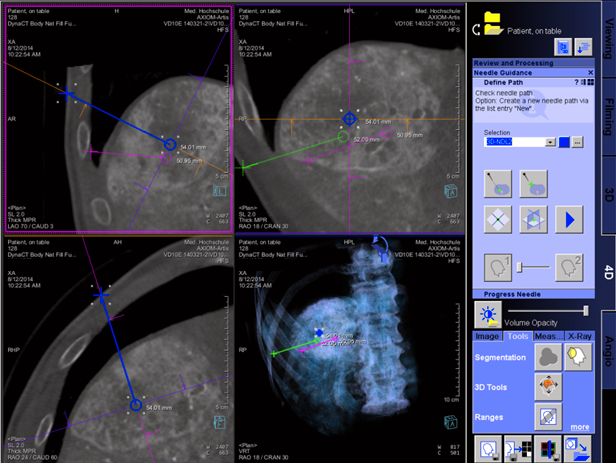
Image guidance and post-procedural imaging for RFA
- RFA cancer treatment overall is safe and efficient
- Complication rate and cost are often lower than in resection
- Treating tumors near major blood vessels, the diaphragm, bowl loops, or major bile ducts may reduce efficacy or pose a risk
- Placing the needle and applying the high energy used in radio frequency ablation relies on image guidance
- Minimize risk of intestinal perforation/penetration of the stomach, duodenum, or colon with high-precision imaging
- Preclude potential deterioration of liver function by the intervention based on high-precision imaging
- At the end of the RFA-cancer treatment procedure, again post-procedural contrast-enhanced CT or MRI is used
- Understanding immediate therapy response remains a challenge
- To better understand the effects of therapy and it’s efficacy, cutting edge imaging technologies like diffusion weighted MRI or PET are often applied
- Detect and manage severe complications using imaging modalities
- Perform follow-up imaging at different intervals, depending on tumor location, histology, and risk of incomplete treatment

Siemens angiography and advanced applications provide an excellent support during RFA procedures:
- Outstanding diffusion-weighted imaging (DWI) reduces blurring and susceptibility to artifacts and high-resolution 3D imaging with reduced breath-hold times with MRI applications
- Integrated cross-hair laser light makes needle procedures with syngo Needle Guidance easy and convenient while saving dose
- Enhance your clinical capabilities with CT-image guided therapy with a hybrid OR

